CMS TEAM Model Explained: How It Works
OnCare360
Dec 27, 2025
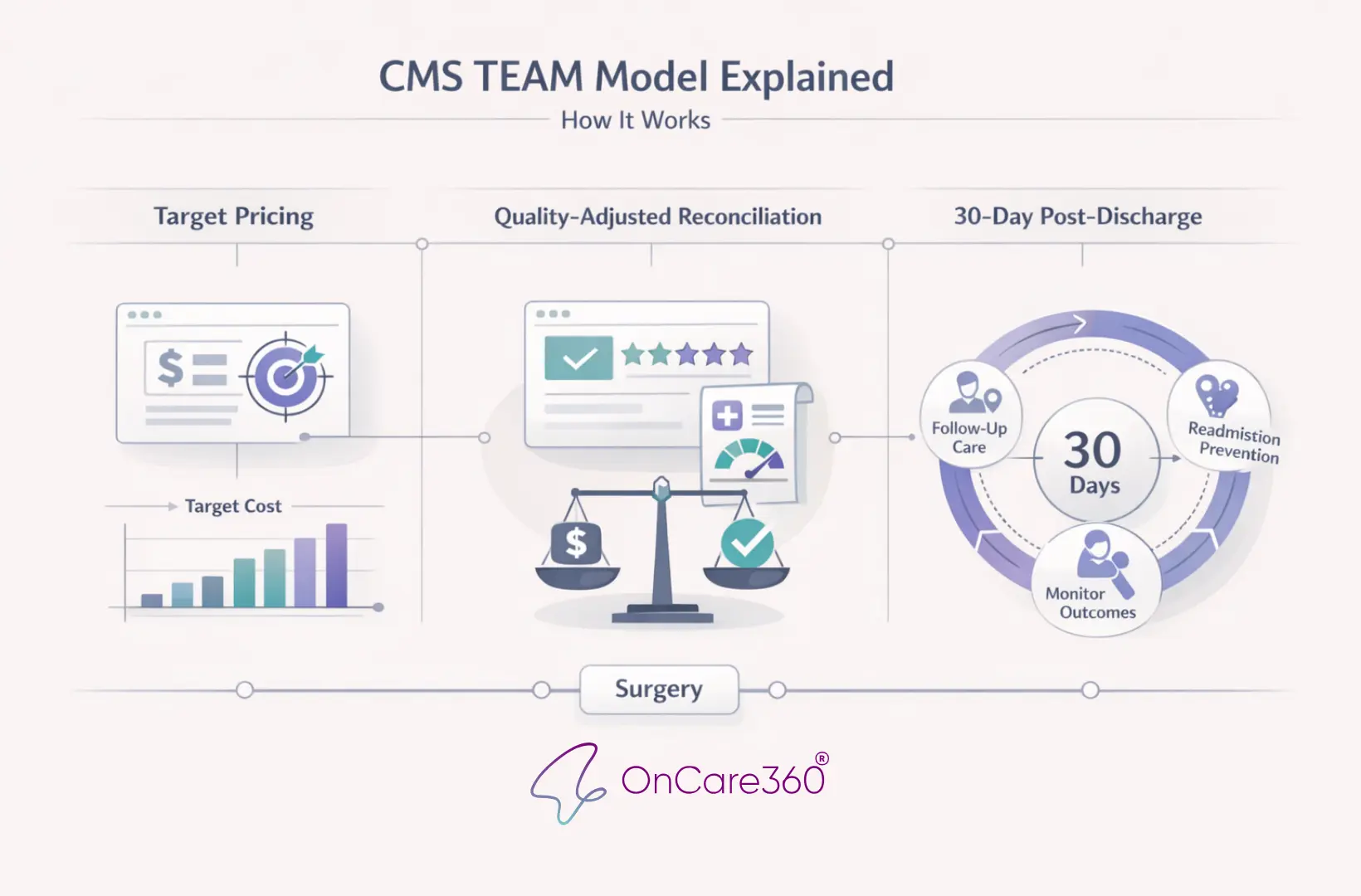
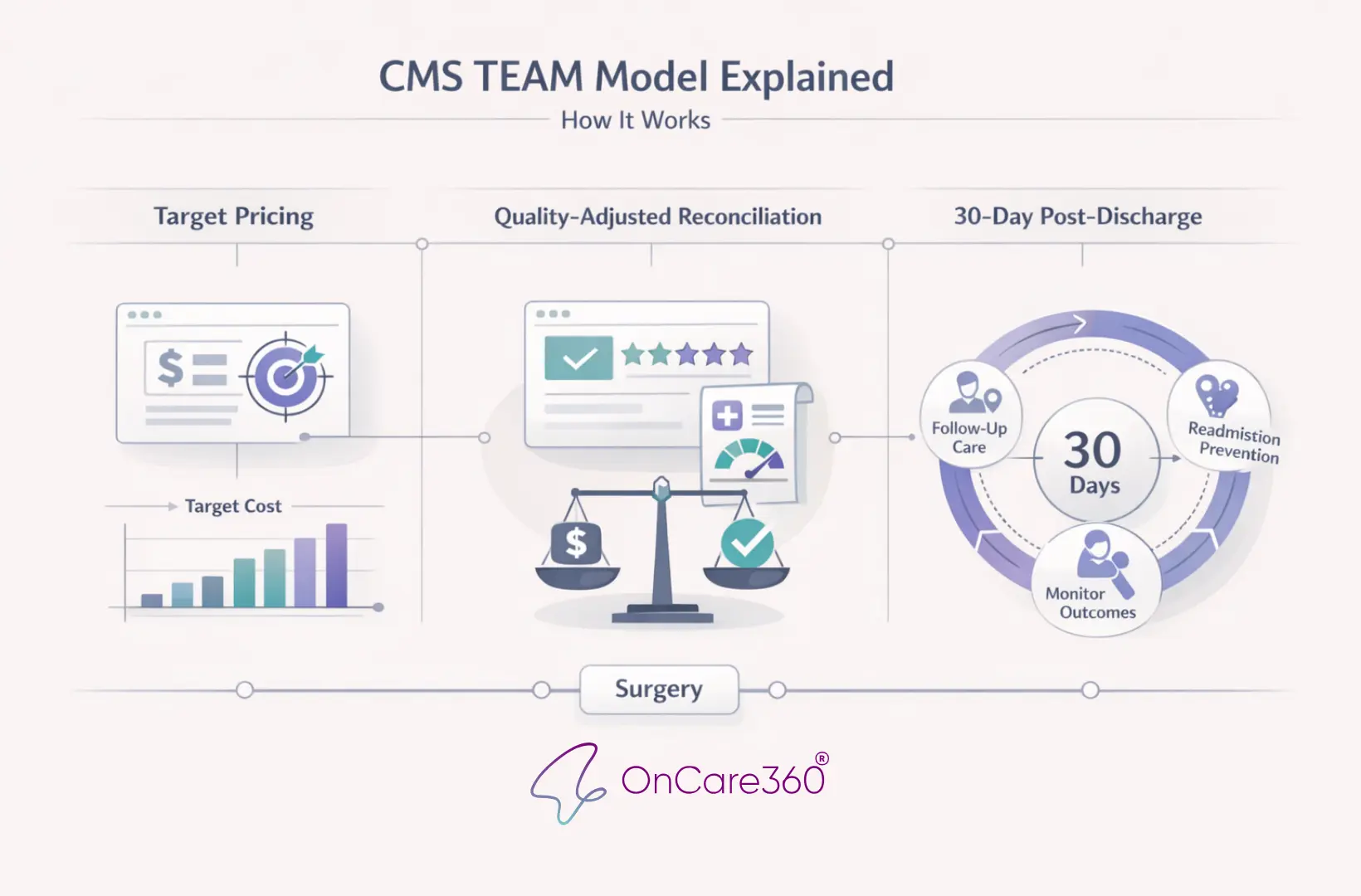
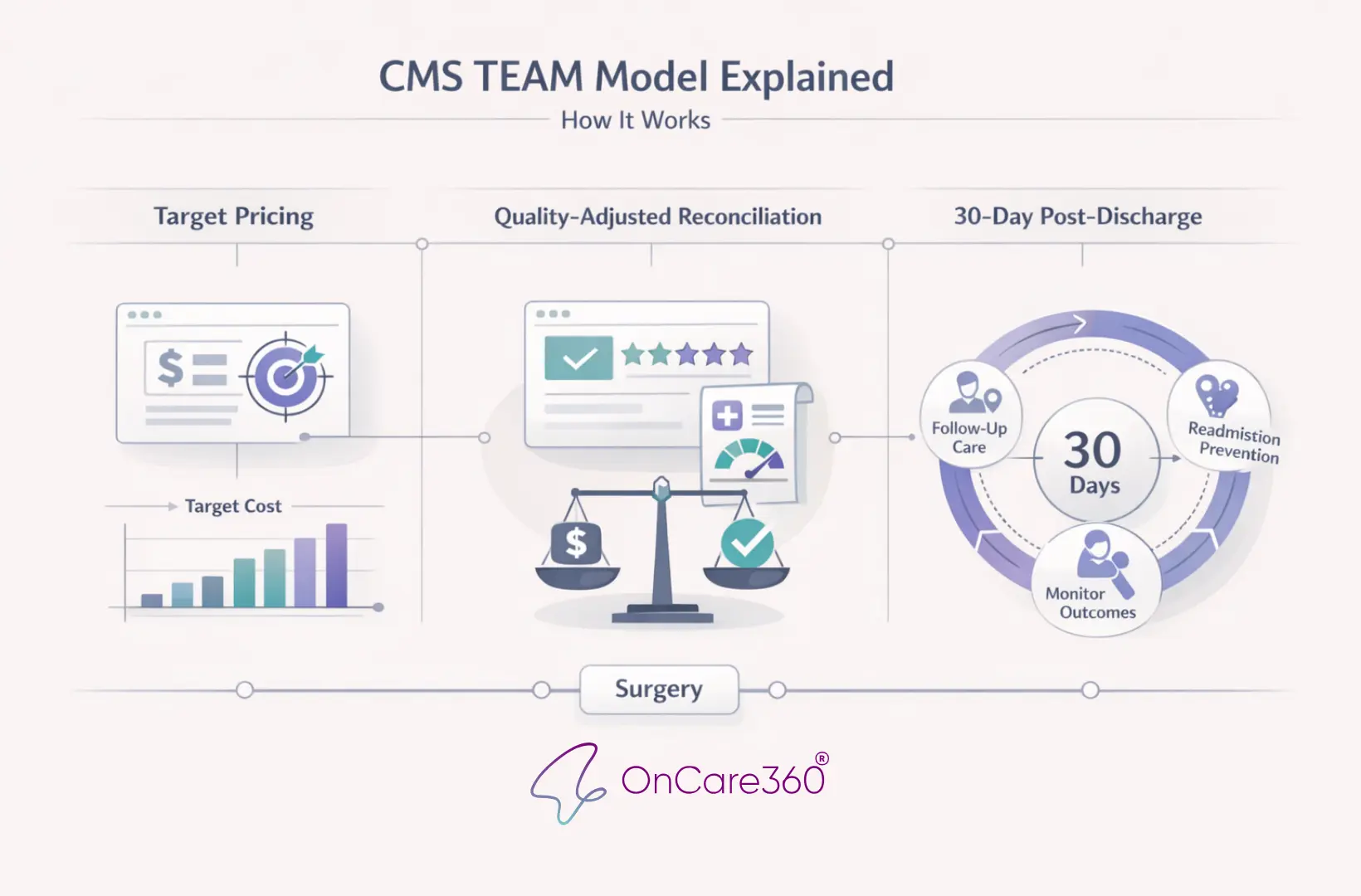
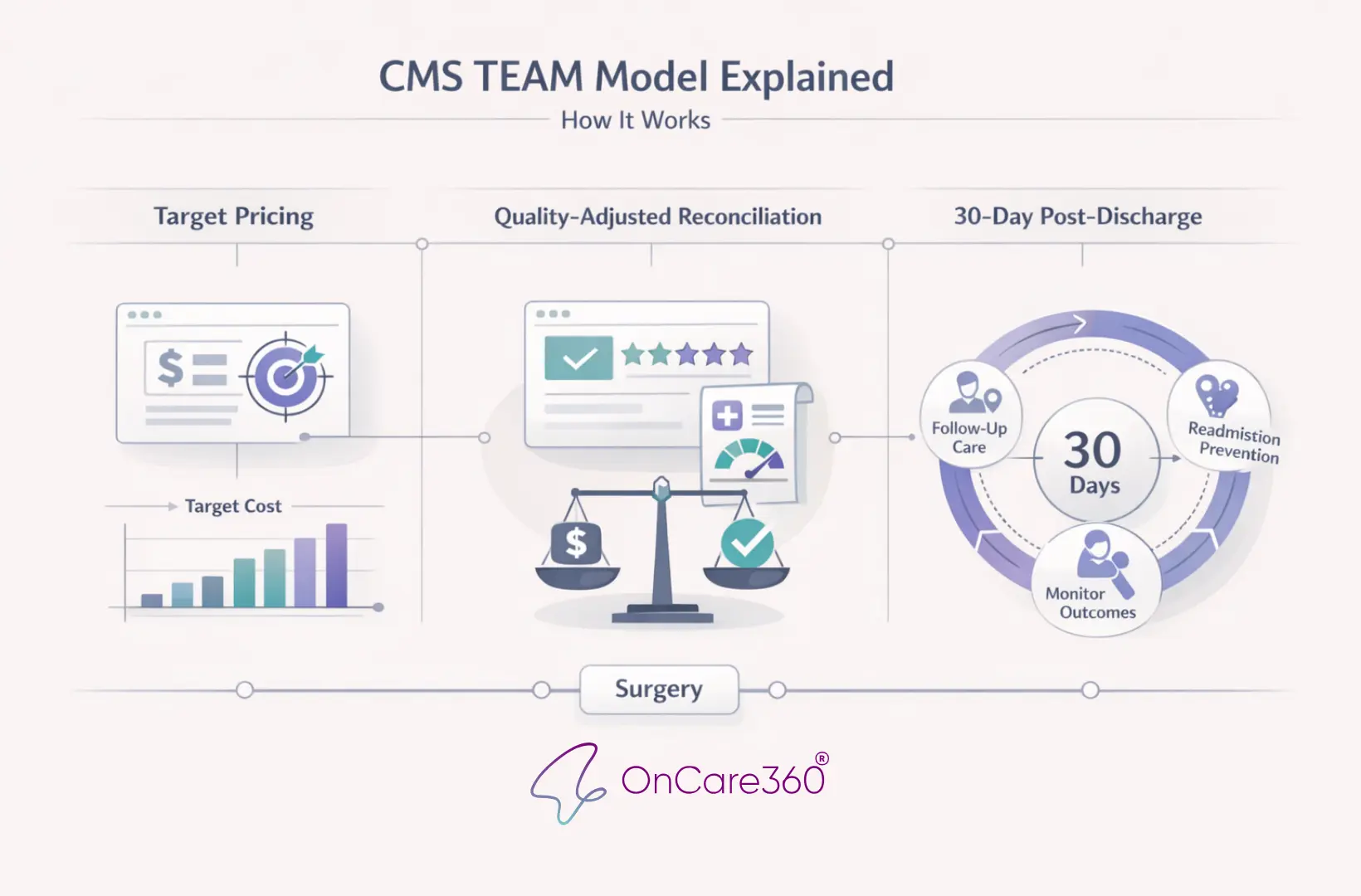
The CMS TEAM Model (Transforming Episode Accountability Model) is a mandatory payment program launching January 1, 2026, aimed at improving surgical care by bundling costs into "episodes" that include surgery and 30 days of post-discharge care. Covering five high-cost procedures like joint replacements and spinal fusion, it ties hospital payments to both cost control and quality outcomes. Hospitals must meet financial and quality benchmarks, with rewards for efficiency and penalties for overspending. This model emphasizes care coordination, particularly in post-surgical recovery, and introduces safeguards for safety net and rural hospitals. Below, we break down its structure, impact, and implementation strategies.
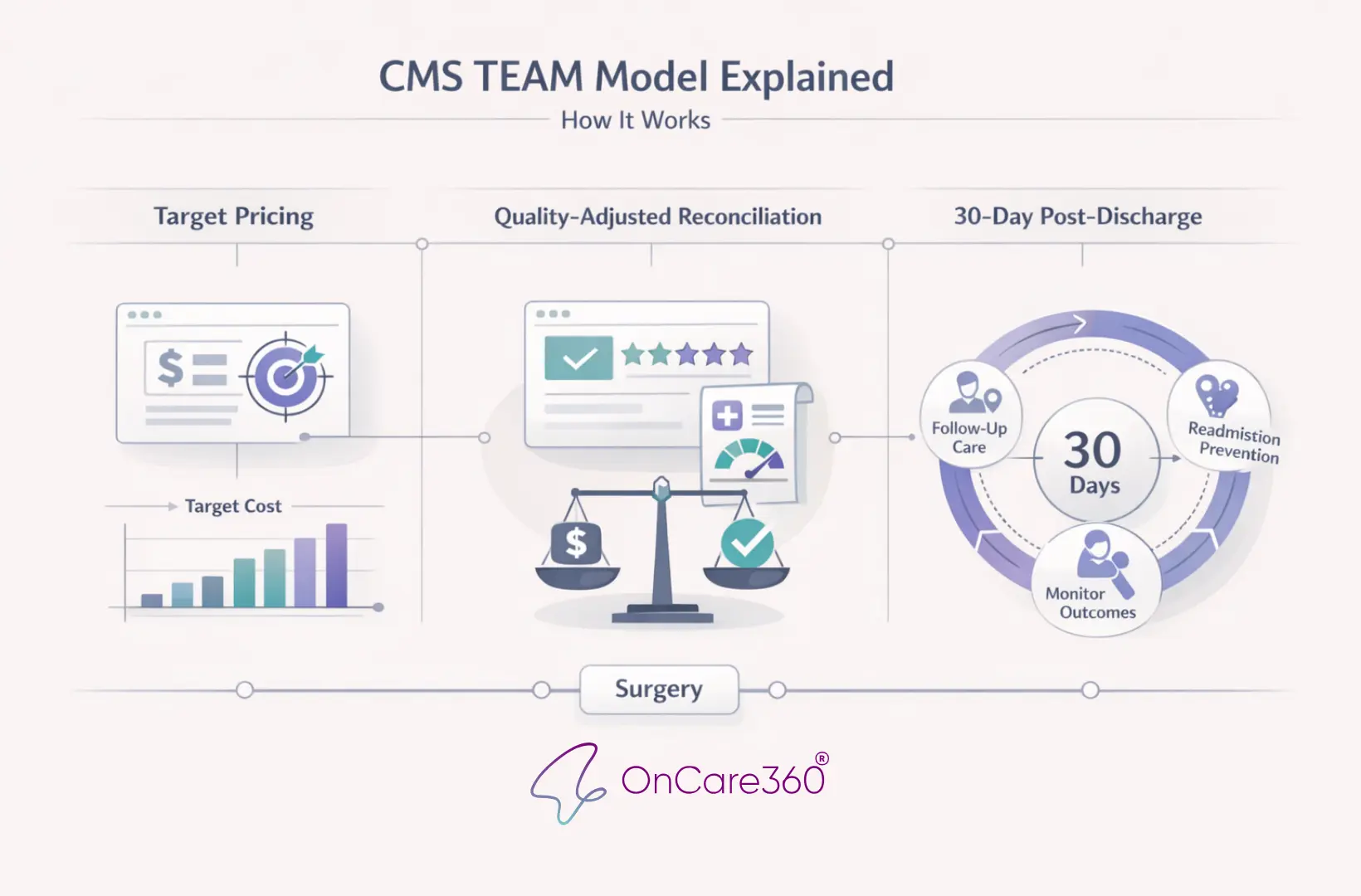
How the CMS TEAM Model Works
The TEAM model establishes a structured approach to managing surgical care by bundling services into defined episodes, setting financial benchmarks based on historical spending, and using quality metrics to measure performance. This framework is designed to hold hospitals accountable starting January 1, 2026.
Covered Surgical Episodes and Scope
The model focuses on five surgical categories: Lower Extremity Joint Replacement (LEJR), Surgical Hip and Femur Fracture Treatment (SHFFT), Spinal Fusion, Coronary Artery Bypass Graft (CABG), and Major Bowel Procedures. Each episode includes all Medicare Parts A and B services, such as surgical fees, post-acute care, and follow-up diagnostics.
Hospitals are responsible for coordinating every aspect of a patient's recovery. For instance, if a patient undergoes a total knee replacement, the associated costs include the orthopedic surgeon’s fees, physical therapy sessions, any necessary readmissions for complications, and follow-up imaging. All these expenses are counted toward the total cost of the episode.
Next, we’ll explore how target pricing and reconciliation processes enforce fiscal accountability.
Target Pricing and Reconciliation Process
The TEAM model ties financial accountability to care quality by setting target prices for each episode. CMS determines these prices using three years of regional spending data, weighted as follows: 17% from the earliest year, 33% from the middle year, and 50% from the most recent year. Adjustments are made for patient complexity, factoring in age, Hierarchical Condition Category (HCC) scores, and socioeconomic indicators like Medicaid eligibility and Community Deprivation Index scores exceeding the 80th percentile.
To ensure Medicare savings, CMS applies discount factors to target prices: 2% for LEJR, SHFFT, and Spinal Fusion procedures, and 1.5% for CABG and Major Bowel Procedures. At the end of each performance year, CMS reconciles actual spending against these discounted targets. Hospitals that keep costs below the target receive financial rewards, while those exceeding the target are required to repay the difference. To protect hospitals from extreme, unpredictable cases, excess costs above the 99th percentile are capped.
This pricing and reconciliation system connects cost management directly to quality outcomes.
Quality Measures and Their Role
Maintaining high-quality care while controlling costs is a cornerstone of the TEAM model. Financial outcomes are adjusted based on quality metrics, with the Composite Quality Score (CQS) playing a central role. The CQS evaluates performance using several metrics, including hospital-wide readmission rates, the CMS Patient Safety and Adverse Events composite, and patient-reported outcomes for hip and knee replacements. Hospitals must collect pre- and one-year post-operative Patient-Reported Outcome Measures (PROMs) for at least 50% of hip and knee arthroplasty patients.
The CQS can modify reconciliation payments significantly - up to a 10% increase for positive performance or a 15% penalty for Track 2 hospitals with poor results. Strong quality scores reduce financial penalties or enhance rewards, while weak performance increases liabilities. This ensures hospitals prioritize both efficiency and patient outcomes, striking a balance between cost control and high standards of care under the TEAM model.
How to Implement the CMS TEAM Model
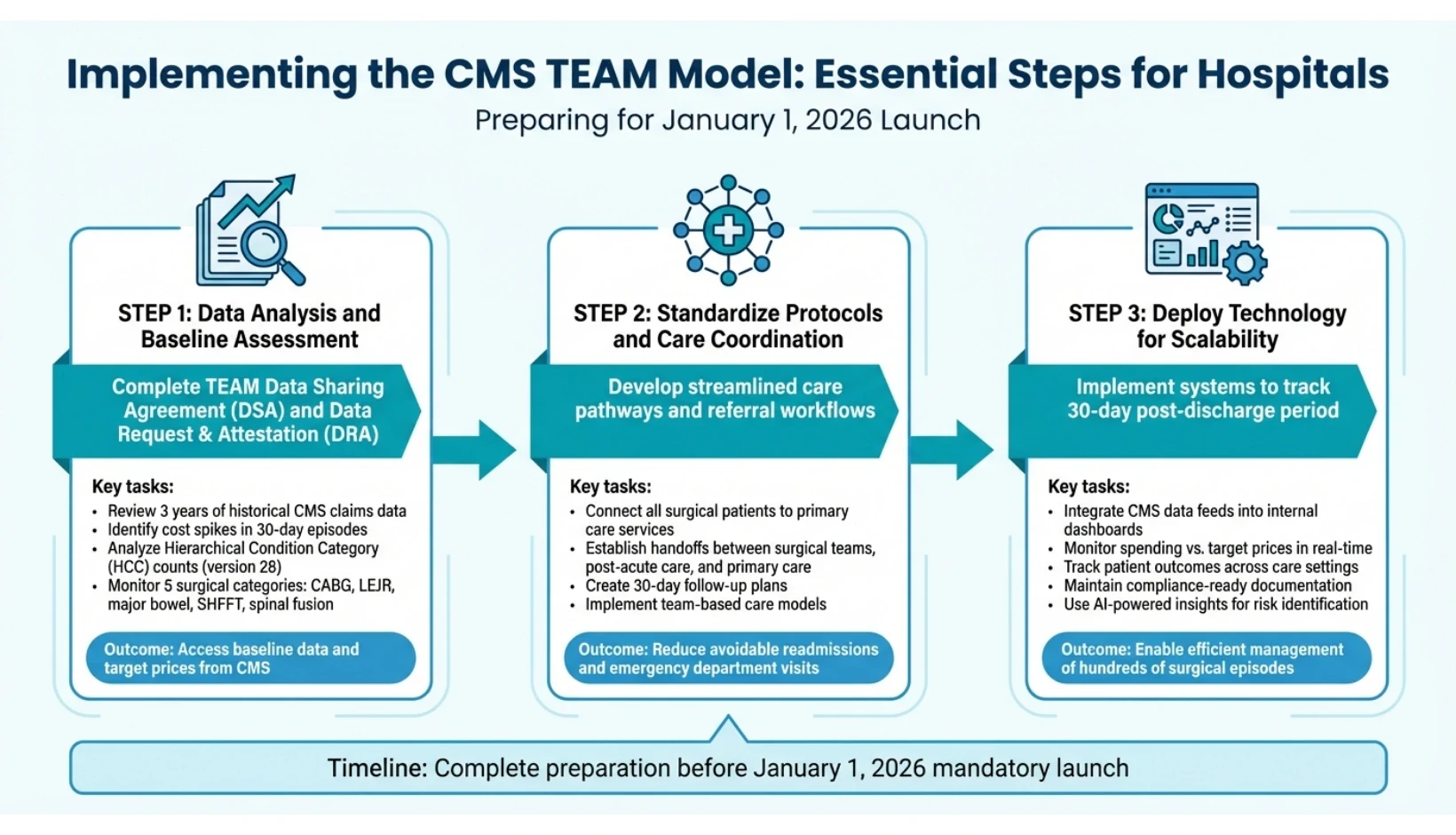
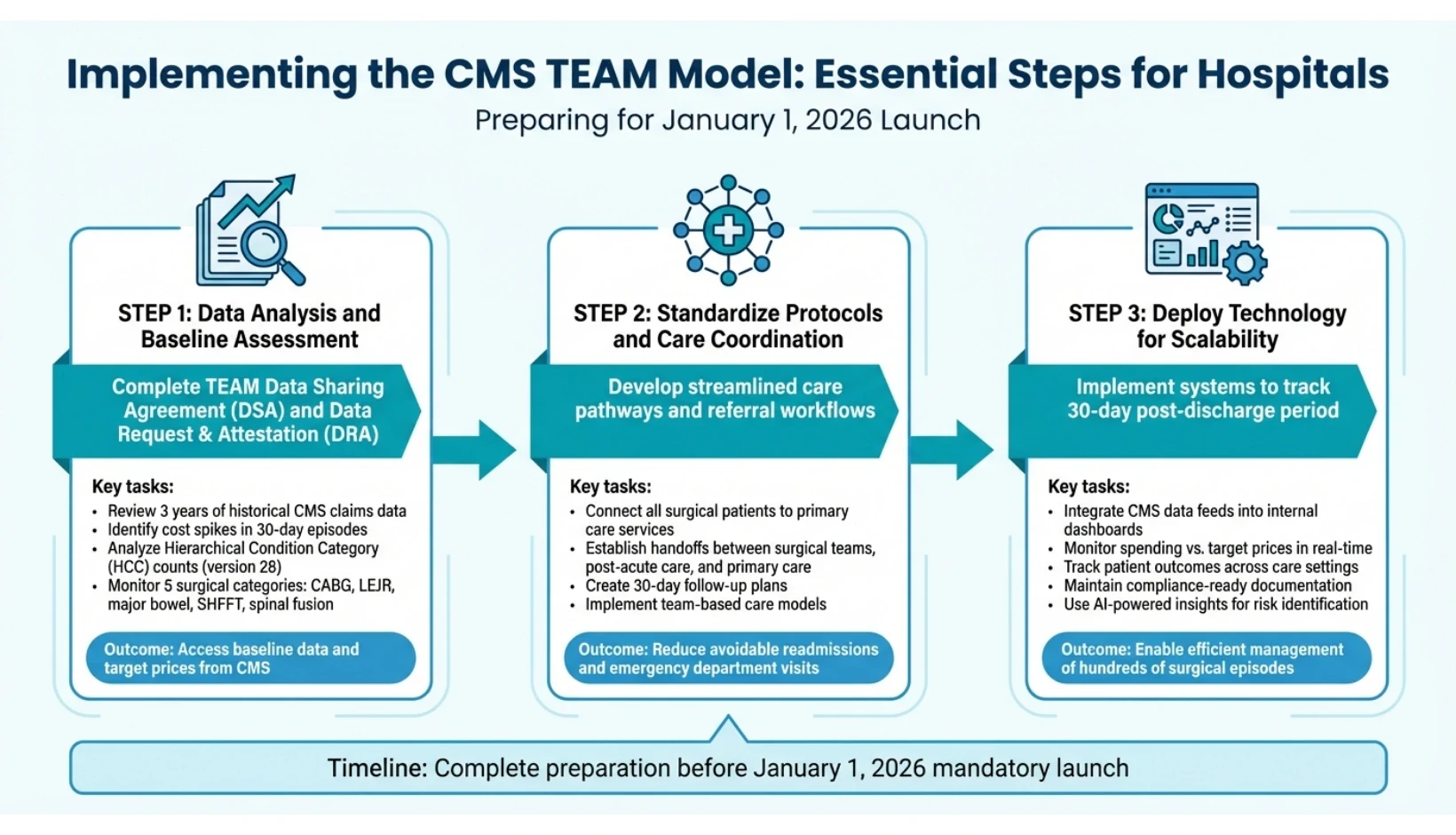
CMS TEAM Model Implementation: 3-Step Hospital Preparation Guide
Implementing the TEAM model effectively requires hospitals to undertake detailed administrative preparation, review historical spending trends, and establish clear accountability for care delivery from surgery through the 30-day post-discharge period. Below are the essential steps to guide hospitals through this process.
Data Analysis and Baseline Assessment
To begin, hospitals must complete the TEAM Data Sharing Agreement (DSA) and Data Request and Attestation (DRA) before the January 1, 2026, launch. These agreements are essential for accessing baseline data and target prices. The baseline data, drawn from three years of historical CMS claims, highlights cost spikes during the 30-day episode - whether due to avoidable readmissions, emergency department visits, or gaps in post-acute care transitions.
A thorough analysis of this data helps pinpoint high-cost drivers across the five surgical categories: CABG, LEJR, major bowel procedures, SHFFT, and spinal fusion. Special attention should be given to Hierarchical Condition Category (HCC) counts from version 28, as these directly influence risk-adjusted target prices. Once the DRA is submitted, CMS may provide monthly performance data, enabling hospitals to monitor and adjust strategies in real time.
Standardizing Protocols and Care Coordination
The TEAM model requires that all patients undergoing covered surgeries be connected to primary care services to ensure ongoing care beyond the 30-day episode. This necessitates the development of streamlined referral workflows and well-defined handoffs between surgical teams, post-acute care providers, and primary care physicians. Standardized care pathways should focus on reducing avoidable readmissions and emergency department visits, as these directly impact both quality metrics and overall costs.
Efforts to improve care coordination should emphasize smooth transitions from acute care to post-acute settings, such as skilled nursing facilities or home health services. Establishing a consistent 30-day follow-up plan - including scheduled provider visits and patient navigation support - is critical. Utilizing team-based care models ensures that all providers within the "medical neighborhood" are aligned on the patient’s recovery plan, reflecting the TEAM model's focus on value-based care and improved outcomes.
Using Technology for Scalability
Technology plays a key role in implementing standardized protocols and ensuring scalability. Hospitals need systems that can track patients across the 30-day post-discharge period, monitor spending relative to target prices, and maintain compliance-ready documentation. While CMS offers general guidance, hospitals are responsible for choosing technology solutions that integrate CMS data feeds into internal dashboards. This enables teams to identify cost drivers and care gaps, allowing for timely adjustments before annual reconciliations.
Platforms like OnCare360 support TEAM model implementation by offering a unified care management system. This platform tracks patient outcomes, coordinates between-visit care, and ensures compliance documentation. With AI-powered insights, it identifies risks based on HCC scores and social determinants, while human oversight ensures clinical decisions are patient-centered. This blend of technology and clinical expertise enables hospitals to manage hundreds of surgical episodes efficiently while maintaining personalized care for each patient.
How OnCare360 Supports the CMS TEAM Model
OnCare360 offers hospitals a centralized platform to manage the crucial 30-day post-discharge period required by the TEAM model. By combining Transitional Care Management (TCM), Chronic Care Management (CCM), and Remote Patient Monitoring (RPM) into a unified workflow, the platform addresses the primary goal of the Centers for Medicare & Medicaid Services (CMS): ensuring surgical patients are connected to primary care services while reducing care fragmentation that often leads to preventable readmissions.
Unified Care Management Platform
The TEAM model holds hospitals responsible for all Medicare Part A and Part B costs within the 30-day post-hospitalization period across five surgical categories: coronary artery bypass grafting (CABG), lower extremity joint replacement (LEJR), major bowel procedures, spinal fusion, and surgical hip/femur fracture treatment (SHFFT). OnCare360 simplifies this responsibility by automating transitions between acute and post-acute care settings. The platform ensures follow-up visits are tracked, primary care referrals are logged, and discharge planning protocols are standardized.
Instead of juggling separate systems for TCM, CCM, and RPM, OnCare360 integrates these programs into a single operational framework. This allows care coordinators to monitor patients recovering from surgeries like spinal fusion or joint replacement while simultaneously managing chronic conditions such as diabetes or heart failure. With 35-40% of hospital readmissions occurring within the first seven days post-discharge, proactive care during this 30-day window is critical for achieving both quality outcomes and financial goals. Effective care transitions remain a cornerstone for meeting TEAM model standards.
AI-Powered Insights and Risk Stratification
OnCare360 enhances care coordination with advanced analytics, using AI-powered tools to identify high-risk patients during the recovery period. The platform prioritizes these patients by analyzing Hierarchical Condition Category (HCC) version 28 counts, clinical data, and Social Determinants of Health (SDOH). This risk stratification aligns with the TEAM model’s risk-adjusted pricing, which accounts for factors like age, HCC scores, and the Community Deprivation Index for beneficiaries in the upper 80th percentile.
Real-time dashboards provide care teams with a clear view of Medicare spending relative to target prices, enabling them to identify cost outliers before the annual reconciliation process. Automated alerts flag patients at risk of readmission, prompting timely interventions. Lisa Fry, Chief Strategy and Innovation Officer at SCP Health, emphasizes the importance of communication:
"Success depends on effective communication systems that coordinate care across multiple providers while keeping patients engaged throughout recovery".
The platform’s predictive analytics also assist hospitals in managing financial performance under the TEAM model’s discount rates - 1.5% for CABG and major bowel procedures, and 2% for LEJR, SHFFT, and spinal fusion. By identifying patients likely to exceed target prices early in the 30-day period, care teams can adjust treatment plans to control costs while maintaining high care standards.
Audit-Ready Compliance and Documentation
Strict compliance with CMS guidelines is a key component of the TEAM model, including adherence to § 512.586 record retention rules, mandatory beneficiary notification letters, and documented primary care referrals. OnCare360 simplifies compliance by automating the generation of standardized notification letters, tracking their delivery, and managing referral workflows.
The platform ensures audit-ready documentation throughout the 30-day post-discharge period, covering time tracking, communication logs, and updates to care plans. This documentation is vital for financial reconciliation, as CMS compares actual spending against risk-adjusted target prices annually. Additionally, OnCare360 supports precise HCC version 28 coding by ensuring clinical documentation accurately captures the risk factors that influence target pricing, such as age and the Community Deprivation Index. These streamlined compliance processes integrate seamlessly with TEAM model requirements, making financial reconciliation more efficient.
Key Takeaways and Future Implications
Benefits of the CMS TEAM Model
The CMS TEAM model shifts away from fragmented fee-for-service payments, introducing an episode-based accountability framework aimed at reducing unnecessary services and avoidable readmissions within a 30-day post-hospitalization period. A mandatory referral to primary care ensures patients receive continued, coordinated care throughout their recovery.
This financial accountability encourages healthcare organizations to invest in better infrastructure, redesign care delivery processes, strengthen post-acute care networks, and utilize real-time data analytics. For safety net hospitals, the model includes a gradual approach to risk, allowing up to three years of upside-only participation before requiring full downside risk. Additionally, quality performance adjustments - up to 10% for positive reconciliation and 15% for negative reconciliation - help ensure cost-saving efforts do not compromise patient safety. These operational changes are paving the way for broader adoption of value-based care.
Preparing for Future Value-Based Care Models
TEAM serves as a stepping stone for future value-based care initiatives. According to CMS, "if the planned TEAM is effective, it may open the door for managing episodes as a standard practice in Traditional Medicare". The model's three-track system allows organizations to develop the operational capacity needed to handle downside risk, easing the transition to more advanced value-based care models.
The infrastructure investments tied to TEAM - such as improved data interoperability, expanded care teams, standardized referral workflows, and robust 30-day post-discharge support - create a solid foundation for success in future CMS programs. Organizations that excel in episode-based care management under TEAM will be better equipped to handle new models that extend accountability periods, include additional clinical categories, or adjust risk parameters.
While the transition to this model presents challenges, industry leaders agree that the potential rewards - better patient outcomes, reduced readmissions, and financial incentives - make the effort worthwhile.
FAQs
How does the CMS TEAM Model improve patient care and manage healthcare costs?
The CMS Transforming Episode Accountability (TEAM) Model aims to improve patient care while managing costs by making hospitals financially responsible for the entire surgical episode. This includes everything from the pre-operative visit to 30 days post-discharge. Payments are tied to quality measures such as care coordination, patient safety, and patient-reported outcomes. Hospitals that meet these quality benchmarks and stay under the spending target can receive financial incentives, whereas those that exceed the target may incur penalties.
This approach pushes providers to refine workflows, cut unnecessary services, and prioritize preventing complications. For patients, the benefits include more coordinated and safer care, fewer readmissions, and quicker recoveries. At the same time, Medicare reduces expenses for high-cost, high-volume surgeries, leading to better results for both patients and the broader healthcare system.
How can hospitals prepare for implementing the CMS TEAM Model?
Hospitals looking to get ready for the CMS TEAM Model should start by familiarizing themselves with its framework and requirements. This includes reviewing the model’s five-year timeline, which begins on January 1, 2026, and determining which risk track - Track 1, 2, or 3 - best suits their financial situation and patient population. Special attention should be given to the five surgical episodes that form the core of the model: lower-extremity joint replacement, surgical hip-femur fracture, spinal fusion, coronary artery bypass graft, and major bowel procedures. These areas will be central to meeting accountability goals.
The next step is to build a strong care coordination system that ensures smooth transitions during the critical 30-day post-discharge period. This involves creating multidisciplinary care pathways, integrating services like skilled nursing and home health, and improving communication across inpatient, post-acute, and outpatient teams. Tools such as patient navigation systems and platforms for real-time recovery tracking can enhance efficiency and help maintain continuity of care.
Lastly, hospitals should focus on aligning quality reporting and financial systems with CMS standards. This means mapping the model’s quality measures - such as care coordination and patient-reported outcomes - onto existing hospital programs. Systems should be put in place to track spending and outcomes for each episode, and risk-sharing agreements with collaborators can help protect financial performance. Engaging early with CMS resources and technical assistance can provide valuable guidance to ensure compliance and success within the TEAM Model framework.
How does the CMS TEAM Model support rural and safety-net hospitals in overcoming resource challenges?
The CMS TEAM Model offers a supportive framework for rural and safety-net hospitals, easing financial strain during the early years of participation through a graduated-risk structure. For up to three years, these hospitals are shielded from downside financial risk, enabling them to focus on building critical care coordination systems without fear of impacting their cash flow. This approach supports essential investments in areas such as post-acute care services, telehealth follow-ups, and primary care referrals - key strategies to help reduce hospital readmissions.
Additionally, the model promotes nationwide participation, providing these hospitals with access to technical assistance, proven best practices, and tools for quality improvement. By aligning financial incentives with enhanced care coordination, the TEAM Model empowers hospitals to improve patient outcomes, address care gaps, and maintain financial health while adhering to episode-based performance standards.
CMS TEAM Model Implementation: 3-Step Hospital Preparation Guide
Implementing the TEAM model effectively requires hospitals to undertake detailed administrative preparation, review historical spending trends, and establish clear accountability for care delivery from surgery through the 30-day post-discharge period. Below are the essential steps to guide hospitals through this process.
Data Analysis and Baseline Assessment
To begin, hospitals must complete the TEAM Data Sharing Agreement (DSA) and Data Request and Attestation (DRA) before the January 1, 2026, launch. These agreements are essential for accessing baseline data and target prices. The baseline data, drawn from three years of historical CMS claims, highlights cost spikes during the 30-day episode - whether due to avoidable readmissions, emergency department visits, or gaps in post-acute care transitions.
A thorough analysis of this data helps pinpoint high-cost drivers across the five surgical categories: CABG, LEJR, major bowel procedures, SHFFT, and spinal fusion. Special attention should be given to Hierarchical Condition Category (HCC) counts from version 28, as these directly influence risk-adjusted target prices. Once the DRA is submitted, CMS may provide monthly performance data, enabling hospitals to monitor and adjust strategies in real time.
Standardizing Protocols and Care Coordination
The TEAM model requires that all patients undergoing covered surgeries be connected to primary care services to ensure ongoing care beyond the 30-day episode. This necessitates the development of streamlined referral workflows and well-defined handoffs between surgical teams, post-acute care providers, and primary care physicians. Standardized care pathways should focus on reducing avoidable readmissions and emergency department visits, as these directly impact both quality metrics and overall costs.
Efforts to improve care coordination should emphasize smooth transitions from acute care to post-acute settings, such as skilled nursing facilities or home health services. Establishing a consistent 30-day follow-up plan - including scheduled provider visits and patient navigation support - is critical. Utilizing team-based care models ensures that all providers within the "medical neighborhood" are aligned on the patient’s recovery plan, reflecting the TEAM model's focus on value-based care and improved outcomes.
Using Technology for Scalability
Technology plays a key role in implementing standardized protocols and ensuring scalability. Hospitals need systems that can track patients across the 30-day post-discharge period, monitor spending relative to target prices, and maintain compliance-ready documentation. While CMS offers general guidance, hospitals are responsible for choosing technology solutions that integrate CMS data feeds into internal dashboards. This enables teams to identify cost drivers and care gaps, allowing for timely adjustments before annual reconciliations.
Platforms like OnCare360 support TEAM model implementation by offering a unified care management system. This platform tracks patient outcomes, coordinates between-visit care, and ensures compliance documentation. With AI-powered insights, it identifies risks based on HCC scores and social determinants, while human oversight ensures clinical decisions are patient-centered. This blend of technology and clinical expertise enables hospitals to manage hundreds of surgical episodes efficiently while maintaining personalized care for each patient.
How OnCare360 Supports the CMS TEAM Model
OnCare360 offers hospitals a centralized platform to manage the crucial 30-day post-discharge period required by the TEAM model. By combining Transitional Care Management (TCM), Chronic Care Management (CCM), and Remote Patient Monitoring (RPM) into a unified workflow, the platform addresses the primary goal of the Centers for Medicare & Medicaid Services (CMS): ensuring surgical patients are connected to primary care services while reducing care fragmentation that often leads to preventable readmissions.
Unified Care Management Platform
The TEAM model holds hospitals responsible for all Medicare Part A and Part B costs within the 30-day post-hospitalization period across five surgical categories: coronary artery bypass grafting (CABG), lower extremity joint replacement (LEJR), major bowel procedures, spinal fusion, and surgical hip/femur fracture treatment (SHFFT). OnCare360 simplifies this responsibility by automating transitions between acute and post-acute care settings. The platform ensures follow-up visits are tracked, primary care referrals are logged, and discharge planning protocols are standardized.
Instead of juggling separate systems for TCM, CCM, and RPM, OnCare360 integrates these programs into a single operational framework. This allows care coordinators to monitor patients recovering from surgeries like spinal fusion or joint replacement while simultaneously managing chronic conditions such as diabetes or heart failure. With 35-40% of hospital readmissions occurring within the first seven days post-discharge, proactive care during this 30-day window is critical for achieving both quality outcomes and financial goals. Effective care transitions remain a cornerstone for meeting TEAM model standards.
AI-Powered Insights and Risk Stratification
OnCare360 enhances care coordination with advanced analytics, using AI-powered tools to identify high-risk patients during the recovery period. The platform prioritizes these patients by analyzing Hierarchical Condition Category (HCC) version 28 counts, clinical data, and Social Determinants of Health (SDOH). This risk stratification aligns with the TEAM model’s risk-adjusted pricing, which accounts for factors like age, HCC scores, and the Community Deprivation Index for beneficiaries in the upper 80th percentile.
Real-time dashboards provide care teams with a clear view of Medicare spending relative to target prices, enabling them to identify cost outliers before the annual reconciliation process. Automated alerts flag patients at risk of readmission, prompting timely interventions. Lisa Fry, Chief Strategy and Innovation Officer at SCP Health, emphasizes the importance of communication:
"Success depends on effective communication systems that coordinate care across multiple providers while keeping patients engaged throughout recovery".
The platform’s predictive analytics also assist hospitals in managing financial performance under the TEAM model’s discount rates - 1.5% for CABG and major bowel procedures, and 2% for LEJR, SHFFT, and spinal fusion. By identifying patients likely to exceed target prices early in the 30-day period, care teams can adjust treatment plans to control costs while maintaining high care standards.
Audit-Ready Compliance and Documentation
Strict compliance with CMS guidelines is a key component of the TEAM model, including adherence to § 512.586 record retention rules, mandatory beneficiary notification letters, and documented primary care referrals. OnCare360 simplifies compliance by automating the generation of standardized notification letters, tracking their delivery, and managing referral workflows.
The platform ensures audit-ready documentation throughout the 30-day post-discharge period, covering time tracking, communication logs, and updates to care plans. This documentation is vital for financial reconciliation, as CMS compares actual spending against risk-adjusted target prices annually. Additionally, OnCare360 supports precise HCC version 28 coding by ensuring clinical documentation accurately captures the risk factors that influence target pricing, such as age and the Community Deprivation Index. These streamlined compliance processes integrate seamlessly with TEAM model requirements, making financial reconciliation more efficient.
Key Takeaways and Future Implications
Benefits of the CMS TEAM Model
The CMS TEAM model shifts away from fragmented fee-for-service payments, introducing an episode-based accountability framework aimed at reducing unnecessary services and avoidable readmissions within a 30-day post-hospitalization period. A mandatory referral to primary care ensures patients receive continued, coordinated care throughout their recovery.
This financial accountability encourages healthcare organizations to invest in better infrastructure, redesign care delivery processes, strengthen post-acute care networks, and utilize real-time data analytics. For safety net hospitals, the model includes a gradual approach to risk, allowing up to three years of upside-only participation before requiring full downside risk. Additionally, quality performance adjustments - up to 10% for positive reconciliation and 15% for negative reconciliation - help ensure cost-saving efforts do not compromise patient safety. These operational changes are paving the way for broader adoption of value-based care.
Preparing for Future Value-Based Care Models
TEAM serves as a stepping stone for future value-based care initiatives. According to CMS, "if the planned TEAM is effective, it may open the door for managing episodes as a standard practice in Traditional Medicare". The model's three-track system allows organizations to develop the operational capacity needed to handle downside risk, easing the transition to more advanced value-based care models.
The infrastructure investments tied to TEAM - such as improved data interoperability, expanded care teams, standardized referral workflows, and robust 30-day post-discharge support - create a solid foundation for success in future CMS programs. Organizations that excel in episode-based care management under TEAM will be better equipped to handle new models that extend accountability periods, include additional clinical categories, or adjust risk parameters.
While the transition to this model presents challenges, industry leaders agree that the potential rewards - better patient outcomes, reduced readmissions, and financial incentives - make the effort worthwhile.
FAQs
How does the CMS TEAM Model improve patient care and manage healthcare costs?
The CMS Transforming Episode Accountability (TEAM) Model aims to improve patient care while managing costs by making hospitals financially responsible for the entire surgical episode. This includes everything from the pre-operative visit to 30 days post-discharge. Payments are tied to quality measures such as care coordination, patient safety, and patient-reported outcomes. Hospitals that meet these quality benchmarks and stay under the spending target can receive financial incentives, whereas those that exceed the target may incur penalties.
This approach pushes providers to refine workflows, cut unnecessary services, and prioritize preventing complications. For patients, the benefits include more coordinated and safer care, fewer readmissions, and quicker recoveries. At the same time, Medicare reduces expenses for high-cost, high-volume surgeries, leading to better results for both patients and the broader healthcare system.
How can hospitals prepare for implementing the CMS TEAM Model?
Hospitals looking to get ready for the CMS TEAM Model should start by familiarizing themselves with its framework and requirements. This includes reviewing the model’s five-year timeline, which begins on January 1, 2026, and determining which risk track - Track 1, 2, or 3 - best suits their financial situation and patient population. Special attention should be given to the five surgical episodes that form the core of the model: lower-extremity joint replacement, surgical hip-femur fracture, spinal fusion, coronary artery bypass graft, and major bowel procedures. These areas will be central to meeting accountability goals.
The next step is to build a strong care coordination system that ensures smooth transitions during the critical 30-day post-discharge period. This involves creating multidisciplinary care pathways, integrating services like skilled nursing and home health, and improving communication across inpatient, post-acute, and outpatient teams. Tools such as patient navigation systems and platforms for real-time recovery tracking can enhance efficiency and help maintain continuity of care.
Lastly, hospitals should focus on aligning quality reporting and financial systems with CMS standards. This means mapping the model’s quality measures - such as care coordination and patient-reported outcomes - onto existing hospital programs. Systems should be put in place to track spending and outcomes for each episode, and risk-sharing agreements with collaborators can help protect financial performance. Engaging early with CMS resources and technical assistance can provide valuable guidance to ensure compliance and success within the TEAM Model framework.
How does the CMS TEAM Model support rural and safety-net hospitals in overcoming resource challenges?
The CMS TEAM Model offers a supportive framework for rural and safety-net hospitals, easing financial strain during the early years of participation through a graduated-risk structure. For up to three years, these hospitals are shielded from downside financial risk, enabling them to focus on building critical care coordination systems without fear of impacting their cash flow. This approach supports essential investments in areas such as post-acute care services, telehealth follow-ups, and primary care referrals - key strategies to help reduce hospital readmissions.
Additionally, the model promotes nationwide participation, providing these hospitals with access to technical assistance, proven best practices, and tools for quality improvement. By aligning financial incentives with enhanced care coordination, the TEAM Model empowers hospitals to improve patient outcomes, address care gaps, and maintain financial health while adhering to episode-based performance standards.

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?


