CMS Consent Documentation: What Must Be Captured
OnCare360
Dec 31, 2025
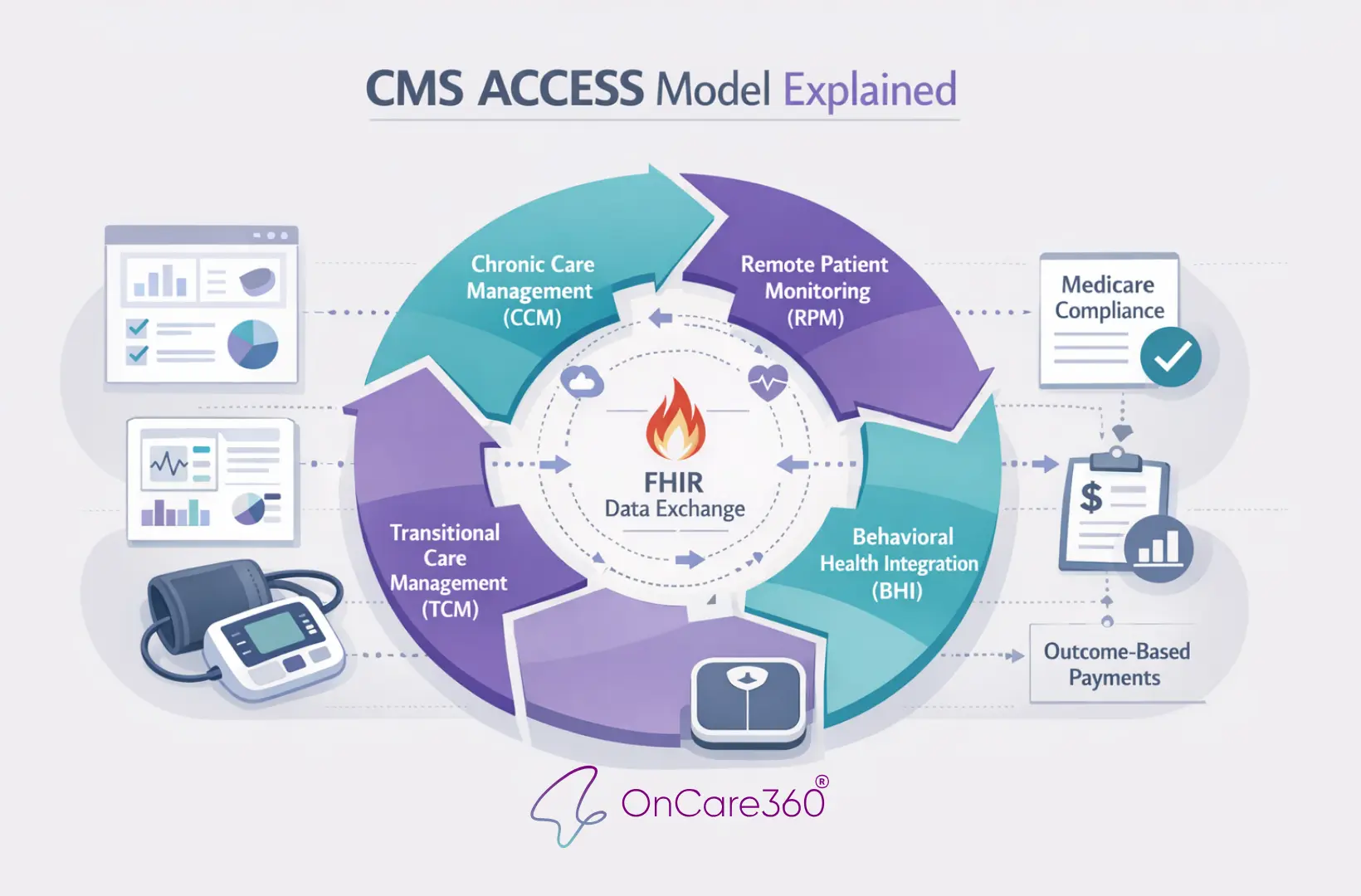
CMS consent documentation is a critical requirement for billing Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Principal Care Management (PCM) services. Without accurate and complete consent, practices risk claim denials, audits, and lost revenue. This article outlines the four required elements for CMS-compliant consent, operational challenges, and strategies to ensure proper documentation.
Physician groups, practice administrators, and value-based care leaders face significant financial and compliance risks if consent forms are incomplete or non-compliant. For example, a single CCM patient can generate over $1,100 annually, but errors in consent documentation can jeopardize reimbursement. The article provides actionable steps to meet CMS standards, avoid legal exposure, and streamline workflows for audit readiness.
Readers will learn:
The four key elements CMS requires for compliant consent
Differences in consent rules for CCM, RPM, and PCM programs
Best practices for verbal vs. written consent documentation
How tools like OnCare360 simplify compliance and audit preparation
Required Elements for CMS-Compliant Consent Documentation
To meet CMS compliance standards, consent documentation must include four key elements: a description of the available services, details on cost-sharing, confirmation that only one provider can bill per month, and acknowledgment of the patient’s right to stop services. These elements must be recorded in the EHR prior to billing, ensuring both compliance and readiness for audits.
Elizabeth Bradford Kneeland, MBA, clarifies the requirements:
The form must spell out program benefits and clinical contact information for the 24/7 care team access. It must state in clear language that participation is voluntary, and there may be out of pocket cost sharing for the patient.
Whether consent is verbal or written, it must document that the patient was informed about the program, understood their financial obligations, acknowledged the single-provider-per-month rule, and was made aware of their right to discontinue services.
Below, each element is explored in detail to guide the creation of audit-ready documentation.
Informing Patients About Available Services
It’s essential to document that patients were informed about the care management program, including specific services like 24/7 access to care, medication management, appointment scheduling, guidance on medication use, and post-hospital follow-up. The explanation should match the actual conversation with the patient.
Corella Lumpkins, a National Advisory Board Member at AAPC, advises:
The summary of the benefits of a CCM program should describe offered services such as: Assistance with scheduling appointments... Guidance for how and when to take medications... [and] Coordination of follow-up care after leaving the hospital.
Be sure to record the date and method of communication in the EHR, noting whether a printed or digital summary was provided to the patient.
Explaining Patient Out-of-Pocket Costs
Patients must be informed about potential costs, including a 20% Medicare coinsurance and applicable deductibles. These cost-sharing requirements apply even for non-face-to-face services. Consent regarding these costs needs to be obtained only once, before services begin. For verbal consent, document in the EHR that the patient acknowledged the costs and agreed to proceed. Additionally, check if the patient qualifies as a Qualified Medicare Beneficiary (QMB), as they may be exempt from these costs. For context, CCM programs save Medicare approximately $74 per patient per month - or $888 annually.
One Provider Per Month Rule
Documentation must clearly state that only one provider can bill for CCM services during a given calendar month. This rule is critical to avoid claim disputes. If two providers submit claims for the same patient in the same month, the claim tied to the consent recorded earlier typically takes precedence. Ask patients if they are currently enrolled with another provider, and document their response. If the patient is switching providers, record the formal revocation of consent with the previous provider to ensure proper billing eligibility for the next month.
Patient's Right to Stop Services
Patients must be informed that they can opt out of the care management program at any time. The revocation becomes effective at the end of the current calendar month. Since CCM consent remains valid until revoked, document both the date of the patient’s request to stop services and the effective date for billing purposes. Ensure the documentation emphasizes that participation is voluntary and withdrawal is allowed at any time.
How to Capture Patient Consent Correctly
When enrolling patients in care management programs, the Centers for Medicare & Medicaid Services (CMS) allows for both verbal and written consent. However, the method you choose can directly influence the clarity of your documentation and your preparedness for audits. Regardless of the format, it's crucial to document the consent in the patient’s medical record before billing. This record must clearly show that all required elements were addressed.
Verbal vs. Written Consent
Verbal consent meets CMS’s minimum requirements for programs like Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Principal Care Management (PCM). It can be obtained and documented by the billing practitioner or auxiliary staff working under their general supervision. Importantly, the medical record must include a detailed note confirming that the patient was informed about all four required elements:
The services available under the program
Cost-sharing obligations
The one-provider-per-month rule
The patient’s right to discontinue services at any time
Corella Lumpkins, an expert from AAPC, emphasizes the importance of thorough consent practices:
Verbal consent is required to enroll patients in the CCM program; however, obtaining written consent is best practice, as is giving the patient a copy of the consent form.
Written consent, on the other hand, offers stronger legal protection and simplifies audit processes. For formal consent under 42 CFR Part 2, it must include specific details such as the patient’s name, authorized individuals, a description of the information disclosed with its purpose, an expiration date or event, and the patient’s signature. Electronic signatures are acceptable unless restricted by local laws. Additionally, providing a physical or digital copy of the signed consent form to the patient is recommended for transparency.
After selecting the consent method, promptly document all relevant details in the electronic health record (EHR) to ensure compliance.
When and Where to Document Consent
Consent should be recorded in the patient’s EHR either at the time services are initiated or before billing occurs. Key details to document include the date of consent and the patient’s decision to enroll. For services like Virtual Check-ins or Communication Technology-Based Services, a single consent can cover a full year. For CCM, the consent remains valid until the patient either revokes it or transitions to a different provider.
Using EHR systems with automated time-stamping is highly beneficial, as it captures the exact date and time of the consent interaction, creating a clear audit trail. If the consent pertains to Substance Use Disorder counseling, it must be captured as a separate written consent and cannot be combined with other medical consents. Additionally, always document whether the patient was provided with a printed or digital summary of the services, as this confirms they were fully informed before agreeing to participate.
How OnCare360 Simplifies Audit-Ready Documentation
Creating audit-ready consent documentation requires structured workflows that ensure all necessary elements are captured, interactions are timestamped, and records are stored in a verifiable format. OnCare360 streamlines this process by automating consent capture and embedding compliance safeguards to minimize the risk of missing documentation. This approach is rooted in established practices for efficient and accurate consent management.
Automated Consent Capture
OnCare360 integrates workflows designed to document all four required CMS consent elements before submitting claims. The platform prompts care coordinators to verify that each of these elements has been completed. By capturing each element as a distinct field within the electronic medical record, OnCare360 reduces the likelihood of errors or omissions that can arise with free-text entries. Additionally, the system automatically logs the date of consent and the patient’s response, ensuring adherence to CMS guidelines.
Time-Stamped Records and Witness Documentation
Beyond capturing consent, OnCare360 timestamps every interaction, creating a reliable audit trail. CMS mandates that consent records be retained for at least 10 years. For oral consent provided via a short form, a witness signature is required on both the form and a summary. OnCare360 addresses this requirement by supporting witness documentation and electronic signatures. The platform also records the care coordinator’s name to meet CMS’s identification requirements. These features collectively strengthen the platform’s alignment with CMS compliance standards, as highlighted throughout this guide.