5-Step Process for Building CMS Audit-Ready Documentation
Creating audit-ready documentation involves a structured approach that integrates every aspect of your between-visit care workflow. It starts with verifying patient eligibility and obtaining proper consent, followed by developing individualized care plans, tracking interactions, applying MEAT criteria, and conducting monthly compliance reviews. Every step must adhere to CMS guidelines while accommodating the specific needs of each patient. The Affordable Care Act mandates that providers establish a compliance program as a prerequisite for Medicare and Medicaid enrollment. These steps not only align with earlier documentation standards but also directly support CMS compliance.
Check Patient Eligibility and Obtain Consent
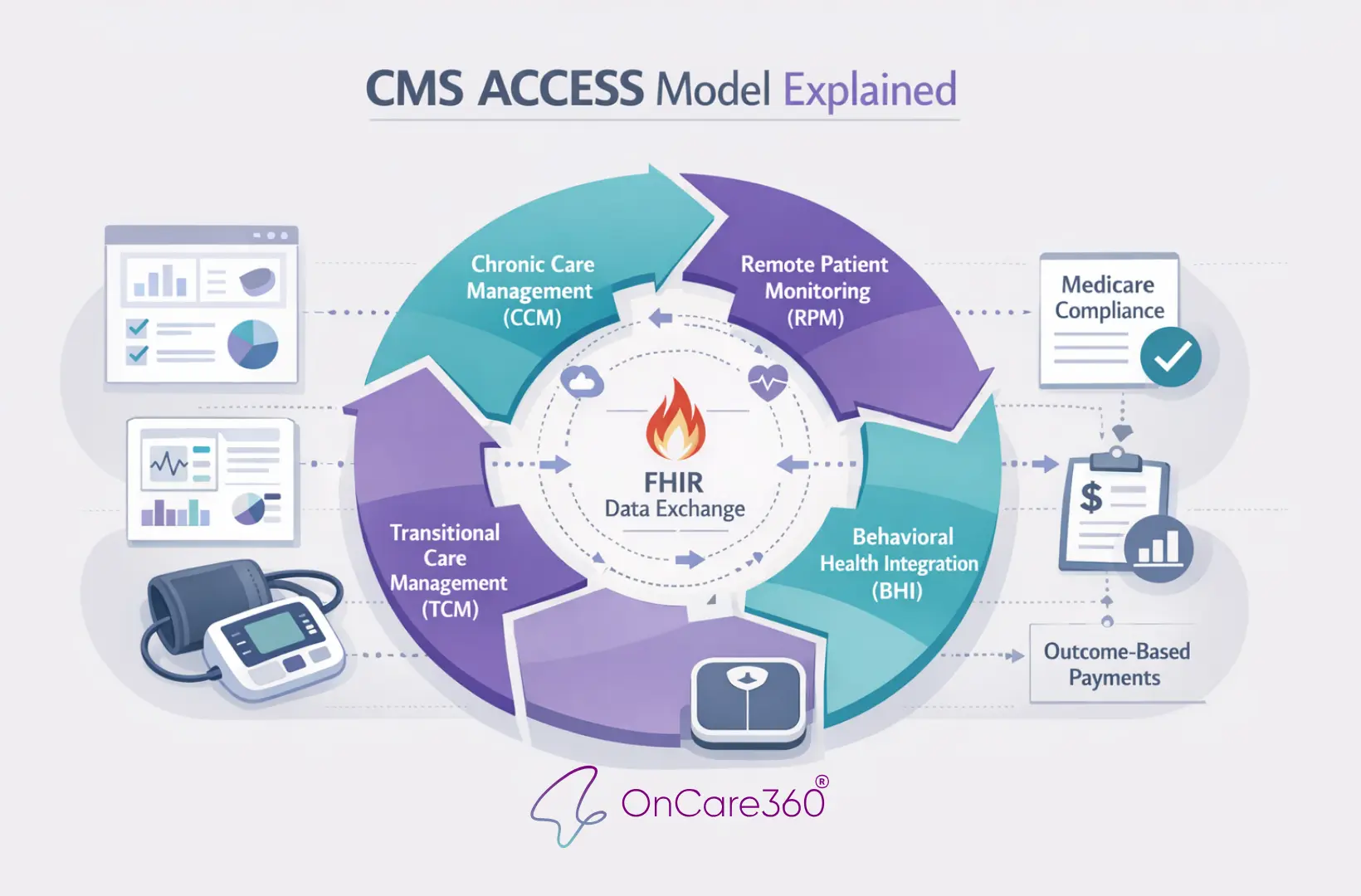
Before initiating services such as Chronic Care Management (CCM), Remote Patient Monitoring (RPM), or Transitional Care Management (TCM), confirm that the patient is enrolled in Medicare Part B and document relevant administrative and data security policies. When securing consent, record essential details like the date, time, and staff member involved, along with all required disclosures. If consent is given verbally, ensure your electronic health record includes an attestation from the staff member confirming the patient understood their cost-sharing responsibilities and their right to opt out.
Incorporate the seven core compliance elements into your workflow: appoint a compliance officer, establish clear communication channels, create written standards of conduct, provide documented staff training, enforce disciplinary measures, conduct internal monitoring, and promptly address detected issues. Keep a log of all compliance training sessions, including timestamps and attendee names, as evidence for audits. CMS emphasizes the importance of training documentation: "Effective practices for a training program include annual training and supporting documentation specifying the date and time of training as well as attendees". This ensures your team consistently applies consent requirements accurately.
Create Patient-Specific Care Plans
CMS evaluates compliance by distinguishing between static elements (fixed requirements like documentation format) and dynamic elements (patient-specific clinical actions) in HCPCS code descriptions. Your care plans should address both, combining the mandated elements with personalized clinical details that reflect the patient’s unique conditions.
When billing for services like G0506 (initial care plan development), ensure your documentation includes a thorough assessment across multiple domains - physical, mental, cognitive, psychosocial, functional, and environmental. Tailor your care plans to the patient’s specific history and current health status, avoiding generic templates. Each plan should clearly narrate the patient’s individual needs and the clinical actions taken to address them.
Record All Interactions with Timestamps
Accurate time documentation is critical for compliance, as CMS requires specific time ranges for services to qualify for payment. Each entry should include the date (MM/DD/YYYY), time range (in 12-hour format with AM/PM), the staff member's name and credentials, duration in minutes, and a description of the clinical activity performed.
For virtual care provided through telecommunications, your notes must demonstrate that all service elements - especially time-based requirements - were met as thoroughly as they would be during an in-person visit. For after-hours calls, document details such as the time of the call, the on-call clinician, call duration, and the clinical guidance provided. This level of detail reinforces your commitment to 24/7 access and ensures every billed minute is substantiated.
Apply MEAT Criteria to Every Diagnosis
Each billed diagnosis must include at least one MEAT (Monitor, Evaluate, Assess, Treat) action, demonstrating individualized clinical decision-making. The documented actions should align with the HCPCS code description and reflect the patient’s unique circumstances during the encounter.
For example, for a patient with Type 2 diabetes (E11.9), hypertension (I10), and hyperlipidemia (E78.5), your documentation might include monitoring diabetes via home glucose log reviews, evaluating hypertension through lab results, and treating hyperlipidemia with medication adjustments. Each diagnosis should have its own MEAT documentation in the encounter note, creating a clear audit trail of active condition management. Summarize these findings in monthly reports to address potential audit gaps proactively.
Create Monthly Audit Summaries
At the end of each month, generate compliance reports to identify and resolve documentation gaps before CMS reviews. Look for missing consent forms, incomplete care plans, insufficient time documentation, or absent MEAT criteria. Regularly review written policies to ensure they meet administrative requirements. Sharing these reports with your team as part of ongoing education helps differentiate compliant practices from areas needing improvement.
Your monthly summaries should include metrics like the total number of enrolled patients, total billable minutes per patient, and the percentage of encounters with complete MEAT documentation. This regular review process allows for timely corrections and demonstrates the effectiveness of your compliance program by showcasing strong internal controls to CMS.
Common Documentation Errors That Trigger Audits
Ensuring compliance with CMS guidelines is essential to avoid audits that can disrupt even well-run care management programs. Common documentation mistakes - such as incomplete consent forms, vague care plans, and insufficient time tracking - can expose your practice to audits, claim denials, and financial penalties. Addressing these issues through standardized workflows is critical for maintaining compliance and operational efficiency.
Missing or Incomplete Consent Forms
One of the most frequent documentation issues involves consent forms. CMS mandates that patients must be informed of key details, including cost-sharing responsibilities, single-provider enrollment, and their right to opt out. Missing essential elements like the date, time, or staff signature can leave claims vulnerable during audits.
Corella Lumpkins, a National Advisory Board Member at AAPC, highlights the importance of thorough documentation:
"Verbal consent is required to enroll patients in the CCM program; however, obtaining written consent is best practice, as is giving the patient a copy of the consent form".
To stay ahead of potential issues, regularly run enrollment reports through your EHR system to verify that every active patient has a complete consent form on file. Written consent is highly recommended to establish a clear audit trail. Additionally, confirm that patients are not enrolled in similar care management services with another provider, as CMS only allows one clinician to bill for these services within a given month.
Generic or Vague Care Plans
Care plans that rely too heavily on templates or macros often fail to meet CMS standards. Auditors expect care plans to include detailed, patient-specific information that reflects each individual's unique conditions and treatment goals. Using identical language across multiple patients or failing to demonstrate tailored clinical actions raises concerns about compliance and program integrity.
CMS provides clear guidance on EHR policies:
"Policies and procedures should address clinical and administrative documentation requirements such as copying and pasting; disabling system features; and how to use templates, macros, and auto-population via default".
To ensure compliance, care plans must balance static elements (standard documentation requirements) with dynamic components that reflect personalized clinical actions. Regular internal reviews can help verify that care plans include specific patient histories, current health conditions, and measurable clinical objectives. Tailoring each care plan not only improves compliance but also enhances the quality of patient care.
Incomplete Time Tracking or Interaction Logs
Accurate time tracking is another critical area where documentation often falls short. For time-based services like CCM, every minute spent on qualifying activities must be precisely documented. Missing or vague time logs are a leading cause of claim denials. CMS treats time documentation as a strict requirement, and any gaps can jeopardize claims.
Time logs should include specific timestamps, staff credentials, detailed descriptions of activities, and the total duration in minutes. Avoid vague language. As the Picmonic Documentation Guidelines note:
"Vague words such as 'appears,' 'seems,' or 'apparently' should be avoided because they convey opinions. Objective data is collected through direct observation, measurements, and patient behavior".
For example, a properly documented interaction might read: "12/28/2025, 2:15–2:32 PM (17 minutes): RN Jane Smith reviewed medication adherence, confirmed metformin use, and discussed side effects." This level of detail not only meets CMS requirements but also provides a clear audit trail. Regularly reviewing monitoring reports can help identify and address incomplete documentation before it becomes a liability.
How OnCare360 Supports Audit-Ready Documentation
OnCare360 streamlines compliance with CMS mandates for consent, care planning, and time documentation by automating critical steps in the workflow. This reduces the risk of audit issues while freeing up clinical staff to prioritize patient care. The platform directly addresses common challenges in documentation through its automation features.
Automated Consent and Eligibility Verification
The platform simplifies patient enrollment by automating the verification of consent and eligibility. Before enrollment, OnCare360 ensures patients meet CMS payment status indicators (A, C, T, or R), reducing the likelihood of claim rejections. Providers can easily comply with CMS requirements for RPM services, such as educating patients and obtaining their consent. The system captures all necessary consent details, including date, time, staff credentials, and acknowledgment of cost-sharing responsibilities. These consent records are centralized for quick access during audits and meet CMS's disclosure requirements.
Customizable Care Plans Aligned with CMS Standards
OnCare360 provides tools to create personalized care plans using the SMART goal framework - Specific, Measurable, Achievable, Relevant, and Time-bound - to effectively track patient progress. The platform supports comprehensive care planning by identifying chronic conditions, developing detailed treatment strategies, and offering educational resources. Each care plan includes CMS-required elements: thorough assessments, current problem lists, treatment plans, medication details, and resource directories. These digital care plans can be shared with other providers and patients through secure portals, ensuring accessibility and transparency. As CMS highlights, "CCM is a critical component of primary care that contributes to better health and care for individuals".
Automatic Time Tracking and Communication Logs
OnCare360 eliminates the need for manual time entry by automatically recording interactions with precise timestamps, staff credentials, activity details, and durations. The platform logs all forms of communication - whether calls, emails, or clinician coordination - in real time, creating a detailed audit trail. This ensures providers meet CMS's time-based documentation requirements for CCM, RPM, and TCM services.
Ready-to-File Audit Reports
By combining automated tracking and care planning, OnCare360 generates comprehensive, CMS-compliant reports ready for audits. The platform organizes consent forms, care plans, time logs, and encounter notes into structured, verifiable reports, reducing reliance on external auditors. These reports include all necessary details to support claims during audits, helping practices avoid penalties or repayment demands. Additionally, the system's efficient reporting improves clean-claim rates, speeds up revenue capture, and reduces administrative burdens for practices and revenue cycle management teams.
Conclusion
Accurate and thorough documentation is the backbone of protecting revenue and safeguarding against CMS audits and potential revenue clawbacks. Adhering to CMS documentation standards - such as detailed time tracking, well-structured care plans, and clear patient consent - ensures an audit-ready defense. As CMS highlights, "Documentation requirements or time range requirements" are "static" elements that "must be met to consider the service complete."
The implications of noncompliance are significant, both operationally and financially. Over half of organizations - 51% - failed compliance reviews, leading to corrective action plans, and CMS penalties for repeated violations can reach up to $2,134,831. Beyond penalties, poor documentation increases the likelihood of claim denials and revenue clawbacks, threatening the sustainability of between-visit care programs.
OnCare360 simplifies this complexity by automating critical aspects of the documentation workflow. It captures time for every interaction, generates care plans that align with CMS standards, and ensures digital records are maintained for CCM, RPM, and TCM services. This automation not only reduces the administrative workload but also guarantees consistent compliance with CMS requirements.
To scale between-visit care programs effectively, robust systems are essential for maintaining compliance at higher volumes. OnCare360 provides the infrastructure for growth by ensuring every patient meets eligibility criteria, every interaction is timestamped, and every care plan includes the necessary assessments and treatment goals. This approach secures predictable revenue, minimizes audit risks, and allows clinical teams to dedicate their efforts to improving patient outcomes.
FAQs
What happens if our documentation doesn’t meet CMS standards?
Failing to meet CMS documentation standards can have serious repercussions. The Centers for Medicare & Medicaid Services (CMS) may initiate an audit by requesting a complete review of your organization’s records. If your documentation falls short of their medical necessity and record-keeping requirements, deficiencies could trigger financial penalties. These penalties may include the recoupment of previously reimbursed funds and enforced clawbacks.
In more severe instances, repeated non-compliance could result in civil monetary penalties, heightened regulatory oversight, or even exclusion from Medicare Part A and B programs. Such an outcome could severely impact your ability to bill for Medicare services, posing a significant threat to your organization’s financial health. Ensuring your documentation is consistently accurate and audit-ready is critical to mitigating these risks and maintaining operational stability.
How can healthcare providers ensure their documentation meets CMS's MEAT criteria?
To comply with CMS's MEAT criteria - Medical necessity, Evaluation, Assessment, and Treatment - healthcare providers need a well-organized documentation process that captures all four elements for every patient interaction. Begin by documenting the medical necessity clearly. This includes outlining the patient’s chronic conditions, meeting qualifying criteria (such as two or more chronic conditions), and specifying the services rendered.
For the evaluation, include up-to-date patient details like vital signs, changes in symptoms, medication adherence, and any new concerns. Always use the standard U.S. date and time format (MM/DD/YYYY hh:mm AM/PM) to ensure consistency.
The assessment should provide a concise summary of the patient’s condition and its connection to their care plan. Highlight any updates, such as modifications to medications or referrals to other providers. For treatment, document specifics like call durations, telehealth platforms used, educational materials shared with the patient, and planned follow-up steps. Don’t forget to record patient consent in the electronic health record (EHR) to meet compliance requirements.
Incorporating standardized templates that prompt for each MEAT component can streamline this process. Regular internal reviews, such as quarterly mock audits, are also valuable for identifying and addressing any documentation gaps ahead of official audits. By embedding these practices into daily workflows, providers can ensure CMS compliance while efficiently managing and expanding their care programs.
What common mistakes lead to CMS audits, and how can they be prevented?
CMS audits are frequently triggered by gaps or errors in documentation. Typical problems include unsigned or incomplete care plans, missing details in call logs, and consent forms that do not align with CMS requirements. Claims often fall short of demonstrating medical necessity or lack proper physician orders, which can draw attention during an audit. Other risk factors include failing to maintain a comprehensive EHR audit trail, neglecting routine internal reviews, or disregarding CMS guidelines for record retention.
To minimize these risks, adopt checklist-based workflows to ensure every claim is backed by complete and accurate documentation, including signed care plans and patient consent forms. Provide thorough training to staff on how to document interactions clearly and consistently within the EHR. Conduct regular internal audits to identify and fix errors promptly, and strictly adhere to CMS policies for record retention. Taking these proactive steps can help reduce audit risks and strengthen compliance efforts.