How AI Expands Care Coordinator Capacity





OnCare360
Jan 3, 2026
Care coordination is a critical component of managing chronic conditions, yet care coordinators face overwhelming administrative burdens, spending up to 55% of their time on documentation and other non-clinical tasks. This inefficiency not only strains resources but also limits their ability to prioritize high-risk patients, impacting value-based care programs such as Chronic Care Management (CCM) and Remote Patient Monitoring (RPM). AI offers a solution by automating routine tasks, identifying at-risk patients, and streamlining workflows, allowing coordinators to focus on clinical priorities and improve patient outcomes.
This article explores how AI tools enhance care coordination by:
Automating documentation to save time and reduce errors.
Using real-time data for early risk identification and intervention.
Improving patient engagement through personalized follow-ups.
Scaling operations without increasing staff, addressing workforce shortages.




How AI Expands Care Coordinator Capacity: Key Statistics and Impact Metrics
AI-Powered Risk Flagging and Patient Prioritization
AI is reshaping how care teams identify and respond to patients requiring urgent attention. By analyzing real-time data from cellular monitoring devices alongside clinical records, claims history, and socioeconomic factors, AI eliminates the need for manual chart reviews. Instead, these models assess 144 variables - such as vital signs, medication adherence, emergency department (ED) history, and socioeconomic indicators - to produce risk scores that predict potential hospitalizations. This approach shifts care from reactive crisis management to proactive intervention, enabling teams to focus on patients at the highest risk. Such a proactive framework enhances the timing and effectiveness of interventions.
Between February 2019 and July 2020, UCLA Health implemented an AI-driven Population Risk Model across 48 primary care clinics. This system analyzed data for 400,000 patients, categorizing those with an acute encounter risk above 35% into three tiers: "Highest‑Risk" (top 5%), "High‑Risk" (patients with prior ED or hospital use), and "Rising‑Risk" (those with high predicted risk but low historical utilization). This structured approach led to a 27% decrease in potentially avoidable hospital admissions.
Using Real-Time Patient Data
Cellular monitoring devices play a critical role in remote patient monitoring by automatically transmitting key health metrics - such as blood pressure, weight, glucose levels, and oxygen saturation - to a centralized platform. AI continuously evaluates these data streams, integrating them with electronic health records and claims data to detect early warning signs. For example, a sudden weight gain in a heart failure patient or a consistent rise in blood pressure for someone with hypertension can trigger alerts before the condition escalates into a medical emergency.
By leveraging these continuous data streams, AI enables automated workflows that flag early signs of clinical deterioration and route alerts to the appropriate care team member. For instance, if a patient records elevated blood pressure readings for three consecutive days, the AI can escalate the case to a registered nurse for timely intervention. This seamless integration of real-time monitoring with patient context allows care teams to act with greater precision, often preventing visible deterioration.
Preventing Missed Interventions
Without AI-driven prioritization, coordinators may overlook patients who appear stable but are at high risk. For "Rising‑Risk" patients, proactive outreach - such as following up on missed appointments, addressing open referrals, and ensuring routine care - is linked to a 30% reduction in hospital admissions and a 42% decrease in ED visits.
AI-generated flags also uncover non-clinical barriers that traditional assessments might miss. For example, the system can highlight issues like transportation challenges, medication management complexities, or home safety concerns. This ensures that specialized staff can address these obstacles before they escalate into crises.
Risk Category | Criteria | Assigned Staff | Primary Focus |
|---|---|---|---|
Highest‑Risk | Top 5% of the at‑risk population | RN or LCSW | Clinical review & monitoring |
High‑Risk | >35% risk with prior ED/hospital use | Comprehensive Care Coordinator | Closing care gaps |
Rising‑Risk | >35% risk with low prior utilization | Patient Service Representative | Addressing missed appointments & referrals |
Source: UCLA Health Proactive Care Model
Automated Documentation and Workflow Support
Care coordinators dedicate a significant portion of their workday - between 34% and 55% - to creating and reviewing clinical documentation. This translates into an annual opportunity cost of $90 to $140 billion in the U.S. AI-powered documentation tools aim to reduce this burden by automating the creation of audit-ready notes and recommending next steps, allowing coordinators to focus more on direct patient care. These tools seamlessly integrate with electronic health records (EHRs), capturing patient context, producing compliant documentation, and optimizing workflows for programs such as Chronic Care Management (CCM) and Remote Patient Monitoring (RPM).
Generating Documentation Automatically
Ambient clinical intelligence leverages voice technology to capture conversations and transform them into audit-ready clinical notes. This technology organizes information into standardized formats that meet Joint Commission (JCAHO) and specialty-specific documentation standards. By reducing documentation time by 50% - saving roughly 7 minutes per encounter - these tools also flag errors in real time, such as incorrect laterality or missing billing codes, ensuring accuracy before finalizing notes.
Beyond transcription, AI systems enhance the readability and structure of patient records by converting unstructured nursing notes and free-text data into coherent, standardized formats. As Scott W. Perkins, B.A., explains:
AI tools... could reduce opportunity cost while producing JCAHO-compliant documentation and assisting coding and billing ventures.
Modern AI documentation platforms also adapt to individual clinician preferences over time, maintaining compliance while aligning with each coordinator's unique documentation style. These systems have a tangible impact on clinician well-being: 70% of clinicians report reduced burnout and fatigue, while 3 out of 4 physicians note improvements in documentation quality after adopting ambient AI tools.
For between-visit care programs, AI-generated documentation ensures every patient interaction is captured in detail, meeting audit standards. These systems automatically track care coordination time, update care plans, and maintain compliance logs - key components for CCM and RPM reimbursement. Impressively, 90% of AI-generated notes are submitted within 24 hours, minimizing delays and reducing the risk of insurance denials.
In addition to generating notes, AI enhances workflow efficiency by streamlining follow-up tasks, making care coordination more effective.
Improving Workflow Efficiency
AI's ability to optimize workflows significantly enhances care coordinator capacity, ensuring consistent and high-quality patient management. After each patient interaction, the system analyzes data to recommend follow-up actions and assign tasks. For example, if a patient mentions challenges with medication adherence, the AI might suggest scheduling a pharmacist consultation, ordering a pill organizer, or assigning a follow-up task. These actionable recommendations reduce decision fatigue and streamline operations. Coordinators can rely on the system to draft lab orders, propose medication adjustments aligned with clinical protocols, or flag care gaps for attention. Additionally, voice commands enable quick access to medical histories, setting reminders, or ordering tests without manual input.
Augmented Intelligence technology can generate up to 80% of progress note content automatically. This shift allows care teams to manage higher patient volumes without compromising quality or requiring additional staff.
For teams overseeing large patient panels in CCM and RPM programs, intelligent task management is critical. AI systems create task lists based on patient risk levels, upcoming care milestones, and regulatory requirements. These tasks are then assigned to team members based on their roles and workload. This approach saves clinicians 12–15 minutes daily and administrative staff 18–25 minutes through more efficient task management.
AI-Supported Patient Follow-Up and Engagement
Maintaining consistent communication with patients between visits is a major hurdle in chronic care management. AI-powered tools are stepping in to simplify this challenge by automating follow-ups, sending relevant reminders, and maintaining ongoing communication. These systems leverage real-time data from wearables, claims, and medical records to prompt timely outreach, helping to improve adherence and address care gaps. This automated outreach integrates seamlessly with the customized patient communication strategies outlined below.
Personalizing Follow-Up Communication
AI harnesses data from wearables, sensors, and medical records to craft follow-up messages tailored to each patient's needs and health conditions. For instance, if a patient’s vital signs suggest a potential issue, the system can send personalized coaching tips, educational materials, or alerts to schedule a check-in. AI-driven conversational agents also provide 24/7 support, offering health education adjusted to each patient’s literacy level. This level of personalization has proven impactful - 45% of patients are more likely to follow health advice when it is customized and delivered at the right moment.
The success of AI-driven personalization is well-documented in large-scale studies. For example, the Apple Heart Study, conducted from 2019 to 2025 with over 419,000 participants, used photoplethysmography sensors and machine learning to detect irregular pulses, achieving an 84% positive predictive value for confirmed atrial fibrillation. Similarly, the Fitbit Heart Study included 455,699 participants and demonstrated 98.7% sensitivity for atrial fibrillation episodes lasting more than 30 minutes, alongside a 98% positive predictive value for irregular rhythms.
AI-powered "nurse-in-the-loop" systems take personalization a step further by using digital twins to simulate a patient’s health status and provide feedback aligned with clinical expertise. These systems also support patients post-discharge by using chatbots to reinforce recovery instructions, ensuring patients understand milestones and recognize warning signs. As Ying Du and colleagues emphasize:
"Unlike decision-support engines or passive risk models, engagement-focused systems emphasize human–AI dialogue and habit formation, with personalization and explainability as key levers".
For between-visit care programs, AI adapts communication based on patient behavior, clinical needs, and preferred communication channels - whether through text, email, or voice messages.
While personalized messaging strengthens patient engagement, AI-driven scheduling and reminder systems help minimize missed appointments and improve participation.
Reducing No-Shows and Improving Participation
Automated reminders and AI-enhanced scheduling tools are highly effective in boosting patient involvement in between-visit care. For example, SMS reminders reduce no-show rates to less than 5%, compared to nearly 35% when only email reminders are used. This is significant given that 90% of text messages are read immediately, and 67.3% of patients prefer text messages over phone calls or emails for appointment reminders.
AI enhances these reminders by analyzing historical data, demographics, and social factors to identify patients most at risk of missing appointments or disengaging from care. Based on this analysis, the system sends behavior-specific nudges, such as reminders tied to medication refill patterns or overdue preventive screenings. Integrated scheduling platforms further support this process by sending smart alerts and incentives, ensuring patients access the right care at the right time. Notably, 34% of patients say that personalized alerts based on their activity or claims data would motivate them to engage more with wellness programs.
Two-way communication features allow patients to confirm, cancel, or reschedule appointments in real time via text or voice, eliminating the need for human intervention while reducing the workload for care coordinators. Additionally, 75% of patients trust AI to help them find in-network providers and book appointments, and 76% believe AI can deliver real-time, tailored healthcare experiences.
Scaling Care Coordination with AI Task Management
AI task management is reshaping care coordination by building on advancements in automated documentation and patient engagement. When combined with AI-driven risk flagging and documentation, task management becomes a critical piece of a broader strategy to streamline care coordination. By automating the creation, delegation, and tracking of tasks, AI enables care coordinators to manage larger patient populations without requiring proportional staffing increases. This approach reduces workflow gaps and allows coordinators to focus on high-priority clinical tasks. The result is a shift from reactive care to a more proactive model, enabling healthcare organizations to optimize resources and better manage at-risk patient populations.
Automated Task Creation and Assignment
AI leverages patient data to categorize individuals by risk and assign tasks accordingly. Complex cases are routed to clinical staff, while routine tasks are directed to administrative teams. For example, UCLA Health implemented an AI model to manage 400,000 patients, achieving a 27% drop in preventable hospital admissions and a 7% faster decline in emergency department visits.
These systems also analyze patient interactions and data to generate follow-up tasks with impressive accuracy - improving task precision by over 70%. Regular updates, often every 90 days, ensure that rising-risk patients are identified and addressed before acute care becomes necessary. Ingolv Urnes, CEO of Generated Health, emphasizes the importance of this approach:
"The best outcomes are achieved by leveraging the persistent, systematic follow-up by AI for routine care combined with processes where the human can step in and resolve escalations or simply provide fulfilling human encounters."
This integration of AI into between-visit care programs like Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) allows coordinators to manage larger panels effectively. AI handles routine monitoring and documentation, freeing staff to concentrate on patients requiring urgent clinical attention. By seamlessly assigning tasks based on risk, the system ensures proactive care and timely intervention.
Monitoring Team Performance
AI-powered dashboards offer real-time insights into care delivery metrics, helping teams meet both productivity and quality benchmarks. These platforms track key indicators such as referral closure rates, care plan adherence, and patient outcomes like readmission rates. By aggregating data across workflows, leaders can pinpoint bottlenecks - whether they stem from provider delays or geographic challenges - without the need for manual data extraction.
Automated escalation protocols address urgent issues, such as missed vital sign checks or compliance alerts, by routing them to the appropriate team member for immediate action. This built-in accountability minimizes the risk of overlooked tasks and supports compliance through automated access controls and audit trails. Dr. Arun Chandra, Clinical Lead at Prevounce, highlights the importance of this balance:
"AI can prioritize and suggest actions, but it's the care team that interprets insights and decides on next steps. Care teams need visibility and final judgment, especially for high-acuity patients."
The benefits of AI-driven performance monitoring are tangible. For instance, in 2025, MUSC Health reallocated over 1,300 hours per week to higher-value patient care by integrating intelligent automation into its workflows. Similarly, Castell, Intermountain's population health company, saved 8,360 staff hours in just two weeks by automating payer care gap attestations across its network of 468 providers. These examples underscore how AI enhances efficiency while maintaining high standards of care coordination.
Measuring AI's Impact on Capacity and Outcomes
As healthcare organizations embrace AI to enhance efficiency and streamline care coordination, the next step is to quantify these improvements using measurable metrics. The most practical evaluation frameworks focus on three key areas: productivity gains, patient outcomes, and financial performance. By addressing all three, organizations can illustrate both operational improvements and clinical value. This dual focus is essential for gaining leadership support and demonstrating return on investment (ROI), particularly within value-based care arrangements.
Tracking Productivity and Efficiency Gains
To understand how AI affects productivity, organizations should monitor specific metrics such as per-patient documentation time and after-hours electronic health record (EHR) usage. Additional indicators include the time required to place orders for each patient and the speed of care transitions, such as identifying discharges within 24–48 hours and completing follow-up calls within 7 days.
Staff well-being is another critical area to evaluate. Metrics like cognitive load, exhaustion, depersonalization, and alert override rates provide insight into how AI tools impact workload and stress levels. As Dr. Corinne Isnard-Bagnis of Sorbonne University explains:
"The need to evaluate and oversee AI-generated insights can contribute to cognitive overload, exacerbate stress, and increase the risk of burnout".
On the clinical side, utilization metrics should focus on outcomes like reductions in preventable hospital admissions and emergency department (ED) visits. Studies show that AI can lower these rates by up to 27%. These efficiency-focused metrics lay the groundwork for connecting operational improvements to enhanced clinical outcomes and financial returns.
Assessing Patient Outcomes and Revenue Impact
AI's value extends beyond saving time - it can also improve patient outcomes and financial performance. To measure these effects, organizations should stratify patients by risk levels and track metrics such as care gap closure rates for interventions like cancer screenings and lab orders. Patient satisfaction and health-related quality of life improvements are equally important to assess alongside clinical outcomes.
Financially, value-based care models benefit from multiple revenue streams influenced by AI. Key metrics include increases in billable claims for programs like Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Principal Care Management (PCM). Monitoring improvements in Risk Adjustment Factor (RAF) scores is also critical to ensure appropriate reimbursement for managing patient complexity. For example, in 2025, Jefferson City Medical Group used AI to identify patients overdue for colorectal cancer screenings, completing the task in just 1 hour compared to 50 manual hours. This efficiency helped elevate their Medicare Star Rating from 4.25 to 5.0 while reducing hospital readmissions by 20% for diabetic patients and 15% for those with chronic heart failure.
Labor cost savings are another area to analyze. Compare the cost of manual outreach (around $5.63 per call) with AI-driven interactions, which cost less than $1 per conversation. Additionally, many practices lose over $297,000 in potential CCM revenue due to operational inefficiencies that AI can streamline. Jonathan Meyers, CEO of Seldon Health Advisors, highlights the broader benefits:
"Return on investment in AI should account for less tangible - but no less crucial - benefits like improved coding accuracy, more timely interventions, reduced administrative burden, and higher clinician satisfaction".
To ensure long-term success, organizations should establish comprehensive KPIs that go beyond financial metrics. Include indicators such as physician adoption rates and coding error rates to create a balanced approach that supports sustainable improvements.
Conclusion
AI-powered care coordination represents a transformative shift in how healthcare organizations manage chronic conditions and optimize between-visit care. By automating tasks like documentation, identifying high-risk patients, and streamlining follow-ups, AI equips care coordinators to oversee larger patient panels without compromising care quality or increasing burnout. Studies highlight the impact of these tools, with organizations reporting a 27% drop in preventable hospital admissions and up to a 50% boost in care manager productivity. (For a deeper dive into these metrics, refer to the Measuring AI's Impact on Capacity and Outcomes section.)
These advancements pave the way for a balanced approach that blends technology with human expertise. Success hinges on maintaining a "human-in-the-loop" model, where AI handles data-heavy tasks like risk stratification and administrative work, leaving licensed clinicians free to focus on patient care and decision-making. This balance is particularly crucial given the looming shortage of over 86,000 physicians by 2036 and the alarming statistic that nearly 50% of primary care physicians report burnout.
Within value-based care models, AI helps practices meet quality benchmarks, close care gaps more effectively, and establish steady revenue streams through programs such as Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and the updated APCM codes set to launch in January 2025. For every 5,000 patients managed, organizations can save approximately $80,000 annually in administrative costs.
By integrating these benefits into a single, unified system, platforms like OnCare360 take care coordination to the next level. This platform combines continuous remote monitoring, structured care pathways, and audit-ready documentation in one place. Its AI-driven prioritization tools work alongside certified care teams to enhance adherence, reduce avoidable events, and scale operations efficiently. Such solutions not only improve clinical outcomes but also deliver measurable financial returns, positioning practices for sustainable growth in a value-based healthcare environment.
Ultimately, the move toward AI-enhanced care coordination is about creating a system that empowers care teams to focus on what truly matters: delivering personalized, high-quality care that keeps patients healthier between visits while reducing overall healthcare costs. This approach tackles today’s challenges while building a strong foundation for the future of value-based care.
FAQs
How does AI help care coordinators work more efficiently?
AI tools improve the efficiency of care coordinators by automating tedious tasks such as documentation, pinpointing high-risk patients, and prioritizing follow-ups. By simplifying these processes, AI reduces administrative workloads, enabling care coordinators to dedicate more time to providing personalized, patient-centered care.
In programs like Chronic Care Management (CCM) and Remote Patient Monitoring (RPM), AI plays a key role in enhancing operational management. It helps scale these initiatives, alleviates burnout among care teams, and supports better patient outcomes. Additionally, these advancements align with the shift toward value-based care, ensuring a more streamlined and effective approach to patient management.
How does AI help care coordinators identify high-risk patients?
AI leverages sophisticated data analysis to assess clinical and utilization data, identifying patients who may face a higher risk of adverse health outcomes. This automated process enables care coordinators to concentrate their efforts on these individuals, facilitating timely outreach and early intervention.
Focusing on high-risk patients enhances care quality while minimizing preventable complications, which can lead to significant time and resource savings. This forward-thinking approach is particularly effective for managing between-visit care programs such as Chronic Care Management (CCM) and Remote Patient Monitoring (RPM), where consistent engagement and monitoring are crucial.
How does AI enhance patient engagement and follow-up care?
AI-driven tools are transforming patient engagement for care coordinators by enabling personalized and automated communication. By analyzing data such as recent appointments, medication adherence, and social determinants of health, these tools segment patient populations and deliver tailored messages. Examples include medication reminders, self-care guidance, and follow-up scheduling prompts, sent directly through text, email, or app notifications. This approach keeps patients informed and engaged without increasing the workload for care coordinators.
When it comes to follow-up care, AI leverages predictive models to identify patients at higher risk, allowing for timely, proactive outreach. Routine tasks like scheduling follow-ups, arranging home-monitoring kits, or escalating complex cases to human coordinators can be automated. This not only streamlines workflows but also ensures that high-priority patients receive the attention they need. By reducing manual processes, preventing missed appointments, and mitigating complications, AI contributes to improved care coordination, better outcomes, and greater operational efficiency.
How AI Expands Care Coordinator Capacity: Key Statistics and Impact Metrics
AI-Powered Risk Flagging and Patient Prioritization
AI is reshaping how care teams identify and respond to patients requiring urgent attention. By analyzing real-time data from cellular monitoring devices alongside clinical records, claims history, and socioeconomic factors, AI eliminates the need for manual chart reviews. Instead, these models assess 144 variables - such as vital signs, medication adherence, emergency department (ED) history, and socioeconomic indicators - to produce risk scores that predict potential hospitalizations. This approach shifts care from reactive crisis management to proactive intervention, enabling teams to focus on patients at the highest risk. Such a proactive framework enhances the timing and effectiveness of interventions.
Between February 2019 and July 2020, UCLA Health implemented an AI-driven Population Risk Model across 48 primary care clinics. This system analyzed data for 400,000 patients, categorizing those with an acute encounter risk above 35% into three tiers: "Highest‑Risk" (top 5%), "High‑Risk" (patients with prior ED or hospital use), and "Rising‑Risk" (those with high predicted risk but low historical utilization). This structured approach led to a 27% decrease in potentially avoidable hospital admissions.
Using Real-Time Patient Data
Cellular monitoring devices play a critical role in remote patient monitoring by automatically transmitting key health metrics - such as blood pressure, weight, glucose levels, and oxygen saturation - to a centralized platform. AI continuously evaluates these data streams, integrating them with electronic health records and claims data to detect early warning signs. For example, a sudden weight gain in a heart failure patient or a consistent rise in blood pressure for someone with hypertension can trigger alerts before the condition escalates into a medical emergency.
By leveraging these continuous data streams, AI enables automated workflows that flag early signs of clinical deterioration and route alerts to the appropriate care team member. For instance, if a patient records elevated blood pressure readings for three consecutive days, the AI can escalate the case to a registered nurse for timely intervention. This seamless integration of real-time monitoring with patient context allows care teams to act with greater precision, often preventing visible deterioration.
Preventing Missed Interventions
Without AI-driven prioritization, coordinators may overlook patients who appear stable but are at high risk. For "Rising‑Risk" patients, proactive outreach - such as following up on missed appointments, addressing open referrals, and ensuring routine care - is linked to a 30% reduction in hospital admissions and a 42% decrease in ED visits.
AI-generated flags also uncover non-clinical barriers that traditional assessments might miss. For example, the system can highlight issues like transportation challenges, medication management complexities, or home safety concerns. This ensures that specialized staff can address these obstacles before they escalate into crises.
Risk Category | Criteria | Assigned Staff | Primary Focus |
|---|---|---|---|
Highest‑Risk | Top 5% of the at‑risk population | RN or LCSW | Clinical review & monitoring |
High‑Risk | >35% risk with prior ED/hospital use | Comprehensive Care Coordinator | Closing care gaps |
Rising‑Risk | >35% risk with low prior utilization | Patient Service Representative | Addressing missed appointments & referrals |
Source: UCLA Health Proactive Care Model
Automated Documentation and Workflow Support
Care coordinators dedicate a significant portion of their workday - between 34% and 55% - to creating and reviewing clinical documentation. This translates into an annual opportunity cost of $90 to $140 billion in the U.S. AI-powered documentation tools aim to reduce this burden by automating the creation of audit-ready notes and recommending next steps, allowing coordinators to focus more on direct patient care. These tools seamlessly integrate with electronic health records (EHRs), capturing patient context, producing compliant documentation, and optimizing workflows for programs such as Chronic Care Management (CCM) and Remote Patient Monitoring (RPM).
Generating Documentation Automatically
Ambient clinical intelligence leverages voice technology to capture conversations and transform them into audit-ready clinical notes. This technology organizes information into standardized formats that meet Joint Commission (JCAHO) and specialty-specific documentation standards. By reducing documentation time by 50% - saving roughly 7 minutes per encounter - these tools also flag errors in real time, such as incorrect laterality or missing billing codes, ensuring accuracy before finalizing notes.
Beyond transcription, AI systems enhance the readability and structure of patient records by converting unstructured nursing notes and free-text data into coherent, standardized formats. As Scott W. Perkins, B.A., explains:
AI tools... could reduce opportunity cost while producing JCAHO-compliant documentation and assisting coding and billing ventures.
Modern AI documentation platforms also adapt to individual clinician preferences over time, maintaining compliance while aligning with each coordinator's unique documentation style. These systems have a tangible impact on clinician well-being: 70% of clinicians report reduced burnout and fatigue, while 3 out of 4 physicians note improvements in documentation quality after adopting ambient AI tools.
For between-visit care programs, AI-generated documentation ensures every patient interaction is captured in detail, meeting audit standards. These systems automatically track care coordination time, update care plans, and maintain compliance logs - key components for CCM and RPM reimbursement. Impressively, 90% of AI-generated notes are submitted within 24 hours, minimizing delays and reducing the risk of insurance denials.
In addition to generating notes, AI enhances workflow efficiency by streamlining follow-up tasks, making care coordination more effective.
Improving Workflow Efficiency
AI's ability to optimize workflows significantly enhances care coordinator capacity, ensuring consistent and high-quality patient management. After each patient interaction, the system analyzes data to recommend follow-up actions and assign tasks. For example, if a patient mentions challenges with medication adherence, the AI might suggest scheduling a pharmacist consultation, ordering a pill organizer, or assigning a follow-up task. These actionable recommendations reduce decision fatigue and streamline operations. Coordinators can rely on the system to draft lab orders, propose medication adjustments aligned with clinical protocols, or flag care gaps for attention. Additionally, voice commands enable quick access to medical histories, setting reminders, or ordering tests without manual input.
Augmented Intelligence technology can generate up to 80% of progress note content automatically. This shift allows care teams to manage higher patient volumes without compromising quality or requiring additional staff.
For teams overseeing large patient panels in CCM and RPM programs, intelligent task management is critical. AI systems create task lists based on patient risk levels, upcoming care milestones, and regulatory requirements. These tasks are then assigned to team members based on their roles and workload. This approach saves clinicians 12–15 minutes daily and administrative staff 18–25 minutes through more efficient task management.
AI-Supported Patient Follow-Up and Engagement
Maintaining consistent communication with patients between visits is a major hurdle in chronic care management. AI-powered tools are stepping in to simplify this challenge by automating follow-ups, sending relevant reminders, and maintaining ongoing communication. These systems leverage real-time data from wearables, claims, and medical records to prompt timely outreach, helping to improve adherence and address care gaps. This automated outreach integrates seamlessly with the customized patient communication strategies outlined below.
Personalizing Follow-Up Communication
AI harnesses data from wearables, sensors, and medical records to craft follow-up messages tailored to each patient's needs and health conditions. For instance, if a patient’s vital signs suggest a potential issue, the system can send personalized coaching tips, educational materials, or alerts to schedule a check-in. AI-driven conversational agents also provide 24/7 support, offering health education adjusted to each patient’s literacy level. This level of personalization has proven impactful - 45% of patients are more likely to follow health advice when it is customized and delivered at the right moment.
The success of AI-driven personalization is well-documented in large-scale studies. For example, the Apple Heart Study, conducted from 2019 to 2025 with over 419,000 participants, used photoplethysmography sensors and machine learning to detect irregular pulses, achieving an 84% positive predictive value for confirmed atrial fibrillation. Similarly, the Fitbit Heart Study included 455,699 participants and demonstrated 98.7% sensitivity for atrial fibrillation episodes lasting more than 30 minutes, alongside a 98% positive predictive value for irregular rhythms.
AI-powered "nurse-in-the-loop" systems take personalization a step further by using digital twins to simulate a patient’s health status and provide feedback aligned with clinical expertise. These systems also support patients post-discharge by using chatbots to reinforce recovery instructions, ensuring patients understand milestones and recognize warning signs. As Ying Du and colleagues emphasize:
"Unlike decision-support engines or passive risk models, engagement-focused systems emphasize human–AI dialogue and habit formation, with personalization and explainability as key levers".
For between-visit care programs, AI adapts communication based on patient behavior, clinical needs, and preferred communication channels - whether through text, email, or voice messages.
While personalized messaging strengthens patient engagement, AI-driven scheduling and reminder systems help minimize missed appointments and improve participation.
Reducing No-Shows and Improving Participation
Automated reminders and AI-enhanced scheduling tools are highly effective in boosting patient involvement in between-visit care. For example, SMS reminders reduce no-show rates to less than 5%, compared to nearly 35% when only email reminders are used. This is significant given that 90% of text messages are read immediately, and 67.3% of patients prefer text messages over phone calls or emails for appointment reminders.
AI enhances these reminders by analyzing historical data, demographics, and social factors to identify patients most at risk of missing appointments or disengaging from care. Based on this analysis, the system sends behavior-specific nudges, such as reminders tied to medication refill patterns or overdue preventive screenings. Integrated scheduling platforms further support this process by sending smart alerts and incentives, ensuring patients access the right care at the right time. Notably, 34% of patients say that personalized alerts based on their activity or claims data would motivate them to engage more with wellness programs.
Two-way communication features allow patients to confirm, cancel, or reschedule appointments in real time via text or voice, eliminating the need for human intervention while reducing the workload for care coordinators. Additionally, 75% of patients trust AI to help them find in-network providers and book appointments, and 76% believe AI can deliver real-time, tailored healthcare experiences.
Scaling Care Coordination with AI Task Management
AI task management is reshaping care coordination by building on advancements in automated documentation and patient engagement. When combined with AI-driven risk flagging and documentation, task management becomes a critical piece of a broader strategy to streamline care coordination. By automating the creation, delegation, and tracking of tasks, AI enables care coordinators to manage larger patient populations without requiring proportional staffing increases. This approach reduces workflow gaps and allows coordinators to focus on high-priority clinical tasks. The result is a shift from reactive care to a more proactive model, enabling healthcare organizations to optimize resources and better manage at-risk patient populations.
Automated Task Creation and Assignment
AI leverages patient data to categorize individuals by risk and assign tasks accordingly. Complex cases are routed to clinical staff, while routine tasks are directed to administrative teams. For example, UCLA Health implemented an AI model to manage 400,000 patients, achieving a 27% drop in preventable hospital admissions and a 7% faster decline in emergency department visits.
These systems also analyze patient interactions and data to generate follow-up tasks with impressive accuracy - improving task precision by over 70%. Regular updates, often every 90 days, ensure that rising-risk patients are identified and addressed before acute care becomes necessary. Ingolv Urnes, CEO of Generated Health, emphasizes the importance of this approach:
"The best outcomes are achieved by leveraging the persistent, systematic follow-up by AI for routine care combined with processes where the human can step in and resolve escalations or simply provide fulfilling human encounters."
This integration of AI into between-visit care programs like Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) allows coordinators to manage larger panels effectively. AI handles routine monitoring and documentation, freeing staff to concentrate on patients requiring urgent clinical attention. By seamlessly assigning tasks based on risk, the system ensures proactive care and timely intervention.
Monitoring Team Performance
AI-powered dashboards offer real-time insights into care delivery metrics, helping teams meet both productivity and quality benchmarks. These platforms track key indicators such as referral closure rates, care plan adherence, and patient outcomes like readmission rates. By aggregating data across workflows, leaders can pinpoint bottlenecks - whether they stem from provider delays or geographic challenges - without the need for manual data extraction.
Automated escalation protocols address urgent issues, such as missed vital sign checks or compliance alerts, by routing them to the appropriate team member for immediate action. This built-in accountability minimizes the risk of overlooked tasks and supports compliance through automated access controls and audit trails. Dr. Arun Chandra, Clinical Lead at Prevounce, highlights the importance of this balance:
"AI can prioritize and suggest actions, but it's the care team that interprets insights and decides on next steps. Care teams need visibility and final judgment, especially for high-acuity patients."
The benefits of AI-driven performance monitoring are tangible. For instance, in 2025, MUSC Health reallocated over 1,300 hours per week to higher-value patient care by integrating intelligent automation into its workflows. Similarly, Castell, Intermountain's population health company, saved 8,360 staff hours in just two weeks by automating payer care gap attestations across its network of 468 providers. These examples underscore how AI enhances efficiency while maintaining high standards of care coordination.
Measuring AI's Impact on Capacity and Outcomes
As healthcare organizations embrace AI to enhance efficiency and streamline care coordination, the next step is to quantify these improvements using measurable metrics. The most practical evaluation frameworks focus on three key areas: productivity gains, patient outcomes, and financial performance. By addressing all three, organizations can illustrate both operational improvements and clinical value. This dual focus is essential for gaining leadership support and demonstrating return on investment (ROI), particularly within value-based care arrangements.
Tracking Productivity and Efficiency Gains
To understand how AI affects productivity, organizations should monitor specific metrics such as per-patient documentation time and after-hours electronic health record (EHR) usage. Additional indicators include the time required to place orders for each patient and the speed of care transitions, such as identifying discharges within 24–48 hours and completing follow-up calls within 7 days.
Staff well-being is another critical area to evaluate. Metrics like cognitive load, exhaustion, depersonalization, and alert override rates provide insight into how AI tools impact workload and stress levels. As Dr. Corinne Isnard-Bagnis of Sorbonne University explains:
"The need to evaluate and oversee AI-generated insights can contribute to cognitive overload, exacerbate stress, and increase the risk of burnout".
On the clinical side, utilization metrics should focus on outcomes like reductions in preventable hospital admissions and emergency department (ED) visits. Studies show that AI can lower these rates by up to 27%. These efficiency-focused metrics lay the groundwork for connecting operational improvements to enhanced clinical outcomes and financial returns.
Assessing Patient Outcomes and Revenue Impact
AI's value extends beyond saving time - it can also improve patient outcomes and financial performance. To measure these effects, organizations should stratify patients by risk levels and track metrics such as care gap closure rates for interventions like cancer screenings and lab orders. Patient satisfaction and health-related quality of life improvements are equally important to assess alongside clinical outcomes.
Financially, value-based care models benefit from multiple revenue streams influenced by AI. Key metrics include increases in billable claims for programs like Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Principal Care Management (PCM). Monitoring improvements in Risk Adjustment Factor (RAF) scores is also critical to ensure appropriate reimbursement for managing patient complexity. For example, in 2025, Jefferson City Medical Group used AI to identify patients overdue for colorectal cancer screenings, completing the task in just 1 hour compared to 50 manual hours. This efficiency helped elevate their Medicare Star Rating from 4.25 to 5.0 while reducing hospital readmissions by 20% for diabetic patients and 15% for those with chronic heart failure.
Labor cost savings are another area to analyze. Compare the cost of manual outreach (around $5.63 per call) with AI-driven interactions, which cost less than $1 per conversation. Additionally, many practices lose over $297,000 in potential CCM revenue due to operational inefficiencies that AI can streamline. Jonathan Meyers, CEO of Seldon Health Advisors, highlights the broader benefits:
"Return on investment in AI should account for less tangible - but no less crucial - benefits like improved coding accuracy, more timely interventions, reduced administrative burden, and higher clinician satisfaction".
To ensure long-term success, organizations should establish comprehensive KPIs that go beyond financial metrics. Include indicators such as physician adoption rates and coding error rates to create a balanced approach that supports sustainable improvements.
Conclusion
AI-powered care coordination represents a transformative shift in how healthcare organizations manage chronic conditions and optimize between-visit care. By automating tasks like documentation, identifying high-risk patients, and streamlining follow-ups, AI equips care coordinators to oversee larger patient panels without compromising care quality or increasing burnout. Studies highlight the impact of these tools, with organizations reporting a 27% drop in preventable hospital admissions and up to a 50% boost in care manager productivity. (For a deeper dive into these metrics, refer to the Measuring AI's Impact on Capacity and Outcomes section.)
These advancements pave the way for a balanced approach that blends technology with human expertise. Success hinges on maintaining a "human-in-the-loop" model, where AI handles data-heavy tasks like risk stratification and administrative work, leaving licensed clinicians free to focus on patient care and decision-making. This balance is particularly crucial given the looming shortage of over 86,000 physicians by 2036 and the alarming statistic that nearly 50% of primary care physicians report burnout.
Within value-based care models, AI helps practices meet quality benchmarks, close care gaps more effectively, and establish steady revenue streams through programs such as Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and the updated APCM codes set to launch in January 2025. For every 5,000 patients managed, organizations can save approximately $80,000 annually in administrative costs.
By integrating these benefits into a single, unified system, platforms like OnCare360 take care coordination to the next level. This platform combines continuous remote monitoring, structured care pathways, and audit-ready documentation in one place. Its AI-driven prioritization tools work alongside certified care teams to enhance adherence, reduce avoidable events, and scale operations efficiently. Such solutions not only improve clinical outcomes but also deliver measurable financial returns, positioning practices for sustainable growth in a value-based healthcare environment.
Ultimately, the move toward AI-enhanced care coordination is about creating a system that empowers care teams to focus on what truly matters: delivering personalized, high-quality care that keeps patients healthier between visits while reducing overall healthcare costs. This approach tackles today’s challenges while building a strong foundation for the future of value-based care.
FAQs
How does AI help care coordinators work more efficiently?
AI tools improve the efficiency of care coordinators by automating tedious tasks such as documentation, pinpointing high-risk patients, and prioritizing follow-ups. By simplifying these processes, AI reduces administrative workloads, enabling care coordinators to dedicate more time to providing personalized, patient-centered care.
In programs like Chronic Care Management (CCM) and Remote Patient Monitoring (RPM), AI plays a key role in enhancing operational management. It helps scale these initiatives, alleviates burnout among care teams, and supports better patient outcomes. Additionally, these advancements align with the shift toward value-based care, ensuring a more streamlined and effective approach to patient management.
How does AI help care coordinators identify high-risk patients?
AI leverages sophisticated data analysis to assess clinical and utilization data, identifying patients who may face a higher risk of adverse health outcomes. This automated process enables care coordinators to concentrate their efforts on these individuals, facilitating timely outreach and early intervention.
Focusing on high-risk patients enhances care quality while minimizing preventable complications, which can lead to significant time and resource savings. This forward-thinking approach is particularly effective for managing between-visit care programs such as Chronic Care Management (CCM) and Remote Patient Monitoring (RPM), where consistent engagement and monitoring are crucial.
How does AI enhance patient engagement and follow-up care?
AI-driven tools are transforming patient engagement for care coordinators by enabling personalized and automated communication. By analyzing data such as recent appointments, medication adherence, and social determinants of health, these tools segment patient populations and deliver tailored messages. Examples include medication reminders, self-care guidance, and follow-up scheduling prompts, sent directly through text, email, or app notifications. This approach keeps patients informed and engaged without increasing the workload for care coordinators.
When it comes to follow-up care, AI leverages predictive models to identify patients at higher risk, allowing for timely, proactive outreach. Routine tasks like scheduling follow-ups, arranging home-monitoring kits, or escalating complex cases to human coordinators can be automated. This not only streamlines workflows but also ensures that high-priority patients receive the attention they need. By reducing manual processes, preventing missed appointments, and mitigating complications, AI contributes to improved care coordination, better outcomes, and greater operational efficiency.

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Dec 28, 2025
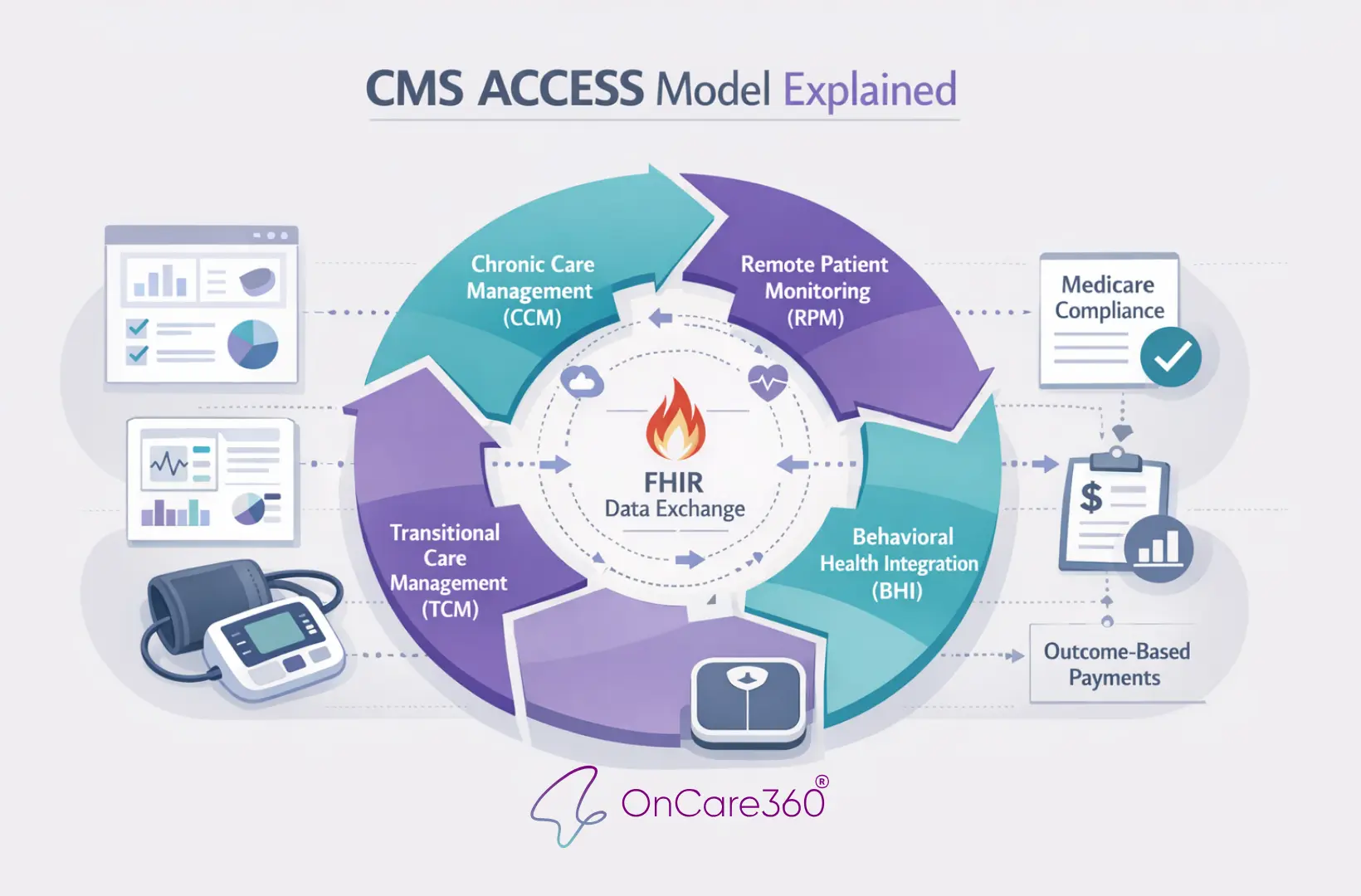
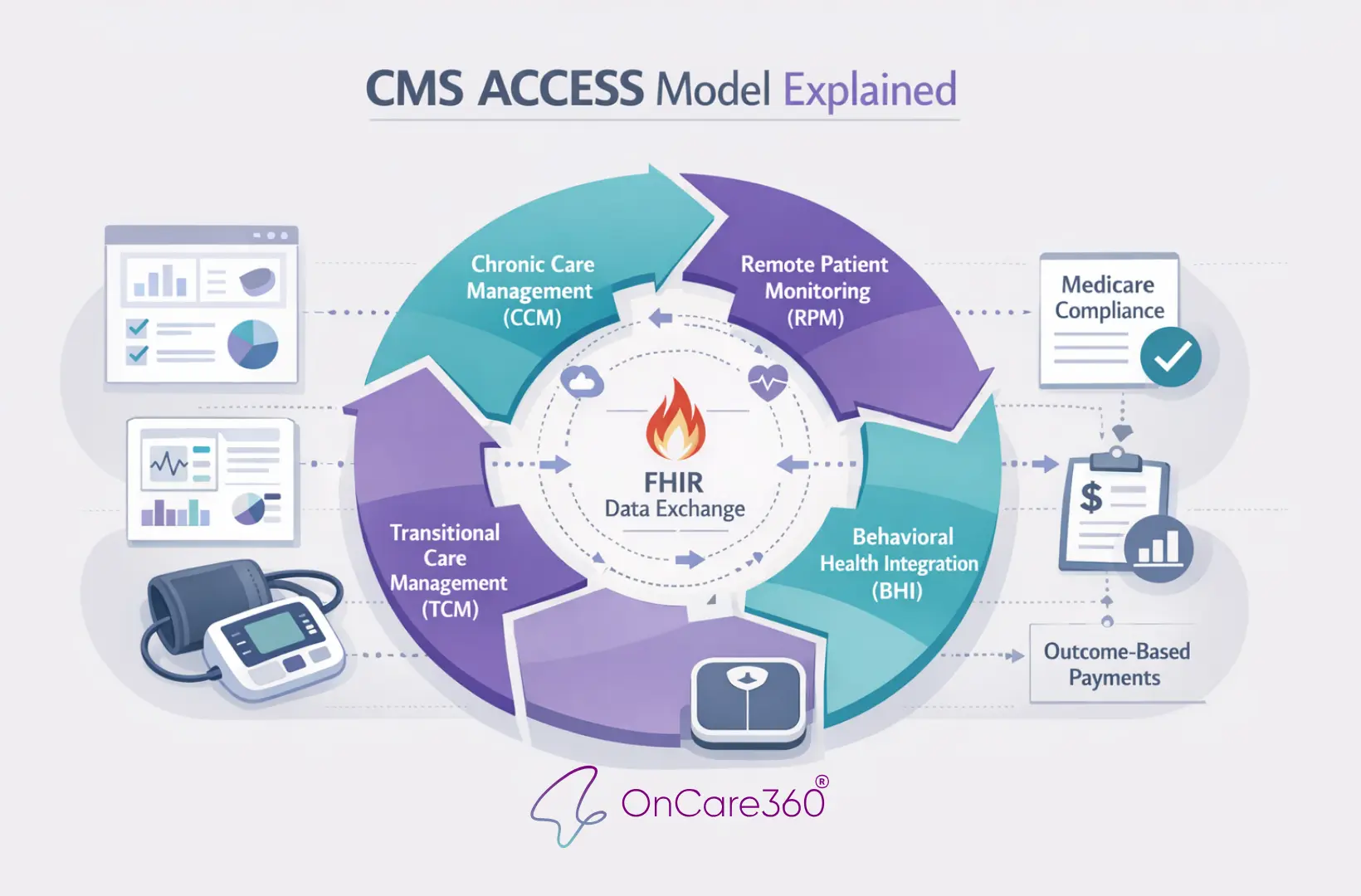
CMS ACCESS Model Explained

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Dec 28, 2025
CMS ACCESS Model Explained
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?


