CMS Updates: How RPM is changing in 2026





OnCare360
Jan 5, 2026
The Centers for Medicare & Medicaid Services (CMS) has introduced critical updates to Remote Patient Monitoring (RPM) policies starting January 1, 2026. These changes include two new CPT codes - 99445 and 99470 - that allow billing for shorter monitoring periods (2–15 days) and reduced management time (10–19 minutes). These updates address operational challenges faced by healthcare providers managing patients with short-term monitoring needs, such as post-surgical recovery or medication adjustments.
These updates simplify RPM billing thresholds, expand reimbursement opportunities, and formalize virtual direct supervision, enabling physicians to oversee care teams remotely via real-time audio-video technology. This article outlines the new billing codes, reimbursement rates, compliance requirements, and operational adjustments needed to align with the 2026 CMS guidelines.
Updated RPM Billing Codes and Reimbursement Rates




2026 CMS RPM Billing Codes: Requirements and Reimbursement Rates
The Centers for Medicare & Medicaid Services (CMS) has introduced two new CPT codes for 2026, aiming to cover clinical work that previously went uncompensated. These codes - 99445 for device supply and 99470 for treatment management - work in tandem with existing Remote Patient Monitoring (RPM) codes, creating a more adaptable billing framework. The 2026 Medicare conversion factor reflects incremental changes for both non-Advanced Payment Model (APM) and qualifying APM participants.
New and Modified CPT Codes
The new CPT 99445 applies to device supply with data transmission for 2–15 days in a 30-day period, while the existing CPT 99454 continues to require at least 16 days. Similarly, CPT 99470 covers the first 10–19 minutes of treatment management within a calendar month, complementing CPT 99457, which remains applicable for 20 minutes or more. CMS has finalized equal reimbursement for device supply codes - both 99445 and 99454 - at approximately $47, reflecting consistent practice expenses regardless of monitoring duration. For treatment management, CPT 99470 is reimbursed at around $26, roughly half the rate of CPT 99457.
Billing teams must select the single code that aligns with the patient’s actual monitoring or management duration. Additionally, all treatment management codes require at least one real-time interactive communication with the patient or caregiver.
CPT Code | Description | Threshold | 2026 Approx. Rate |
|---|---|---|---|
99445 | 2–15 day device supply | 2–15 days / 30 days | ~$47 |
99454 | 16–30 day device supply | 16–30 days / 30 days | ~$47 |
99470 | Treatment management (first) | 10–19 min / month | ~$26 |
99457 | Treatment management (first) | 20+ min / month | ~$52 |
99458 | Treatment management (add-on) | +20 min increments | ~$41 |
99453 | Initial setup and education | One‑time | ~$22 |
These updates address previous gaps in billing thresholds and introduce more precise time requirements for RPM services.
Reduced Time Requirements for RPM Billing
The updated thresholds resolve a critical issue in RPM reimbursement. Data reveals that 16% of patients recorded 2–15 readings, and 6% received 10–20 minutes of clinical staff time - services that previously went unpaid. These patients, often requiring short-term monitoring for medication adjustments, post-surgical recovery, or acute symptom management, were unable to meet the previous benchmarks of 16 days of monitoring or 20 minutes of clinical management.
"By recognizing shorter monitoring windows and smaller time increments, CMS is rewarding meaningful engagement instead of arbitrary thresholds", remarked Vivo Care.
Practices can now bill for patients who record vitals for as few as two days within a 30-day period or who receive a minimum of 10 minutes of clinical management. However, billing teams must carefully track monitoring days and management minutes, as 99445 and 99454 cannot be billed simultaneously for the same patient in the same month.
Changes to Reimbursement Rates
The revised billing structure for 2026 not only simplifies RPM coding but also enhances revenue opportunities by capturing services that were previously uncompensated. For instance, in June 2025, a clinic in Upstate New York managing 522 patients with hypertension and diabetes identified 83 patients (16%) with 2–15 readings and 31 patients (6%) receiving 10–20 minutes of staff time. Under the 2025 rules, these services generated no revenue. With the 2026 updates, the clinic projects an annual revenue increase of $101,124.
CMS is now using the Hospital Outpatient Prospective Payment System (OPPS) Geometric Mean Cost (GMC) data to establish valuations for technical RPM services like device supply codes. This methodology promotes transparency and ensures more predictable rate-setting. Practices can expect care management revenue to grow by an estimated 10% to 20% under the 2026 guidelines.
Daniel Tashnek, JD, Co-Founder and CEO of Prevounce Health, stated: "The 2026 final rule represents a tangible shift toward that goal, pairing clinical flexibility with improved financial stability."
Key considerations for billing teams:
Update EHR and billing systems to differentiate between 2–15 days (99445) and 16–30 days (99454) of data transmission.
Monitor clinical staff time meticulously to determine whether the 10-minute (99470) or 20-minute (99457) threshold is met in a given month.
Document the date, method, and summary of required real-time interactive communication for all treatment management codes.
Confirm that commercial payers have adjusted their fee schedules to include 99445 and 99470, as Medicare adoption does not guarantee immediate alignment from private insurers.
Documentation and Compliance Requirements
The 2026 CMS updates introduce revised billing thresholds, offering more flexibility but requiring meticulous record-keeping to ensure audit readiness. As billing practices evolve, accurate documentation becomes essential for maximizing RPM revenue. Providers must maintain comprehensive records that capture clinical staff activities and all real-time patient interactions. Following a 2024 report highlighting billing discrepancies, the Office of Inspector General is expected to increase scrutiny of RPM claims through audits.
Documentation Standards for Audits
Four key documentation elements are required to support every RPM claim.
First, providers must clearly establish that remote monitoring is medically necessary for diagnosing or treating a specific illness or injury.
Second, practices must maintain daily logs confirming the digital transmission of physiological data from the patient’s device. For CPT 99445, at least two days of data within a 30-day period must be logged, while CPT 99454 requires a minimum of 16 days. Only digitally gathered data satisfies this requirement.
Third, detailed records must include specific dates, staff identities, and total minutes spent on care activities. This supports the time thresholds of 10–19 minutes (CPT 99470) or 20+ minutes (CPT 99457). While voicemails and asynchronous messages can contribute to total care management time, they do not meet the requirement for interactive communication.
Fourth, synchronous communication must be documented. For CPT codes 99470, 99457, and 99458, providers must record the date, method, and a summary of each real-time, two-way interaction. Text messages, voicemails, manual uploads, or AI-generated conversations do not qualify as interactive communication.
"For compliant programs, the message is clear: continue to document thoroughly, use technology that enforces payer rules, and partner only with vendors that maintain strict medical-necessity standards." – Daniel Tashnek, JD, Co-Founder of Prevounce Health
Meeting these documentation standards ensures practices can align with updated supervision and eligibility requirements.
Eligibility and Supervision Rules
In addition to documentation mandates, CMS has clarified supervision and patient eligibility rules. The agency has permanently adopted a definition of direct supervision that allows "immediate availability" through real-time audio-video technology for incident-to services. This means supervising physicians or advanced practitioners are no longer required to be physically present when clinical staff provide RPM services. However, documentation must demonstrate that the supervising practitioner was accessible via live two-way video, as audio-only communication does not meet the interactive communication standard established for 2026.
This virtual supervision model applies to clinical staff, including third-party RPM vendors, working as an extension of the practice. Supervising clinicians retain the authority to determine whether virtual direct supervision is appropriate for patient safety on a case-by-case basis. These updated supervision standards complement the billing and documentation improvements, ensuring smooth operational workflows.
The 2026 updates also broaden patient eligibility criteria. Beyond chronic conditions, RPM services now include post-operative care, sleep disorders, medication titration, and transitional care after hospital discharge. Practices must document the medical necessity for each episode of care. Additionally, when a patient is discharged and later re-enrolled for a new clinical reason, a new patient consent form must be obtained and documented.
Key compliance considerations:
Configure EHR templates to capture the interactive communication summaries required for the new 10-minute management code CPT 99470.
Ensure virtual supervision is conducted using two-way audio-video technology.
Avoid billing CPT 99470 (10–19 minutes) and CPT 99457 (20+ minutes) for the same patient in the same month.
How CMS Updates Affect Operations and Finances
The 2026 updates from CMS bring significant changes to Remote Patient Monitoring (RPM) workflows, creating opportunities for practices to capture additional revenue. By lowering time and monitoring thresholds, these updates open doors for billing services that were previously excluded, while also requiring operational adjustments to ensure compliance and reduce claim denials. Practices that refine their staffing strategies, enhance documentation systems, and adjust patient selection criteria can expect improvements in both clinical outcomes and financial performance.
Adjusting Workflows for Short-Duration Monitoring
With the introduction of CPT 99445, clinical teams can now integrate short-term monitoring into their care plans. This code allows billing for 2–15 days of data transmission within a 30-day period, making it particularly useful for scenarios such as medication titration, post-surgical recovery, or acute care transitions. For example, a patient adjusting diabetes medication after being discharged from the hospital might require monitoring for only two weeks. Under the new guidelines, this generates $47 in device supply reimbursement, which was previously unbillable due to the stricter 16-day requirement.
Additionally, CPT 99470 enables practices to bill for 10–19 minutes of monthly care coordination, valued at $26. This allows for shorter, more frequent patient interactions, eliminating the need to wait for 20 minutes of cumulative management time. To optimize this process, practices should update their EHR systems to flag when patients reach the 10-minute threshold and ensure all synchronous communications are documented. Virtual supervision further supports distributed clinical teams, enabling seamless operations.
"Clinicians can now bill for fewer monthly vital readings and shorter management time. For patients, this means RPM programs can finally match clinical reality." – Daniel Tashnek, JD, Co-founder, Prevounce Health
These updates not only streamline workflows but also provide new avenues for revenue, as explored below.
Effects on Revenue and Claim Denials
The reduced billing thresholds now make it possible to capture revenue for services that were previously excluded. For instance, practices often lost revenue when patients transmitted data for only 10–15 days or when clinical staff spent just 15 minutes on care coordination. The 2026 updates address these gaps, particularly benefiting patients with lower acuity who need less intensive monitoring but still gain from remote oversight.
However, it’s important to note that billing codes are mutually exclusive within a given month. To avoid claim denials, practices should configure billing systems to automatically select the appropriate code based on actual patient engagement data. Although these changes offer greater flexibility, the Office of Inspector General (OIG) continues to closely monitor RPM claims for medical necessity and proper documentation of interactive communication. Regular internal audits are essential to maintain compliance and minimize denials.
2025 Requirement | 2026 New Option | Revenue Impact |
|---|---|---|
Minimum 16 days of data | 2–15 days of data (CPT 99445) | Captures $47 for short-term episodes |
Minimum 20 minutes management | 10–19 minutes management (CPT 99470) | Captures $26 for low-acuity check-ins |
Physical direct supervision | Permanent virtual supervision | Reduces overhead for clinical staff oversight |
These updates not only provide financial benefits but also expand the scope of RPM services to reach more patients.
Serving More Patient Populations
The new CMS guidelines allow practices to extend RPM services to a broader range of patient needs. Beyond chronic conditions, practices can now bill for post-operative care, sleep disorders, medication titration, and transitional care following hospital discharge. This shift toward episodic monitoring reflects real-world clinical scenarios, where patients often need intensive monitoring during specific treatment phases rather than continuous oversight.
Practices should review their patient panels to identify individuals who were previously ineligible for RPM services but now qualify under the updated thresholds. For example, a patient recovering from joint replacement surgery may need only short-term monitoring, which qualifies for CPT 99445 and CPT 99470. Each enrollment must include documented medical necessity for the specific condition being treated. Additionally, if a patient is discharged and later re-enrolled for a different clinical issue, a new consent form is required.
"These new codes empower providers to engage patients more meaningfully and operate programs that are both clinically effective and financially sustainable." – Dr. Kang, CEO, KangarooHealth
Key operational considerations include:
Updating EHR templates to track 2–15 day monitoring windows and 10-minute management increments
Training billing staff on mutually exclusive code pairings to avoid denials
Establishing virtual supervision protocols using real-time audio-video technology
Designing specific clinical pathways for short-term monitoring during medication adjustments and post-discharge recovery
Conducting monthly internal audits to ensure proper documentation of medical necessity for all active enrollments
How to Implement the 2026 RPM Updates
Implementing the 2026 updates to Remote Patient Monitoring (RPM) involves three key steps: auditing your current program, training your team, and expanding services.
Reviewing Your Current RPM Program
Start with a detailed audit of your existing RPM platform to ensure it can handle the updated billing thresholds. The system must differentiate between patients transmitting data for 2–15 days versus 16 or more days, as well as track clinical staff time spent on care coordination - 10–19 minutes versus 20+ minutes. Without these capabilities, you risk billing errors, missed opportunities for reimbursement, or claim denials.
Next, identify patients who now qualify under the updated CPT 99445 and CPT 99470 codes. These include individuals needing short-term medication adjustments, those recently discharged from the hospital, or patients requiring episodic monitoring for acute conditions. These new eligibility criteria open doors to services that were previously unavailable.
Ensure your billing systems are equipped to enforce the mutually exclusive code rules introduced in the updates. Additionally, confirm that your supervision model supports the permanent virtual direct supervision rule. This change allows supervising physicians to meet the "immediately available" requirement through real-time audio-video communication, eliminating the need for physical presence.
Finally, stay informed about payer adoption timelines. While Medicare has finalized these codes for 2026, commercial insurers may implement them on varying schedules. Track which payers in your area have approved coverage for CPT 99445 and CPT 99470 to avoid submitting claims that could be rejected.
Once these audits are complete, the focus shifts to updating electronic health record (EHR) systems and training your staff to integrate the new guidelines effectively.
Staff Training and EHR System Updates
Update your EHR and billing systems to incorporate CPT 99445, which covers 2–15 days of data transmission, and CPT 99470, which applies to 10–19 minutes of care management time. Automate time tracking for patient interactions within this 10–19 minute range to ensure accurate billing and reimbursement.
Train clinical teams on the requirements for virtual direct supervision, proper coding, and real-time documentation. The 2026 rule allowing "direct supervision" through real-time audio-video technology enhances team flexibility and efficiency, especially for distributed care teams. However, adhering to documentation and communication protocols is crucial for compliance.
"The interactive communication contributes to the total time, but it does not need to represent the entire cumulative reported time of the treatment management service." – CMS Final Rule
Highlight the importance of "live, interactive communication" for treatment management codes. Staff must conduct at least one real-time phone or video interaction per month to bill for CPT 99470, 99457, or 99458; text messages or voicemails alone do not meet the requirements. Update EHR templates to include logs for timing and communication, ensuring records are audit-ready, as RPM billing continues to face scrutiny from the Office of Inspector General (OIG).
Tailor monitoring plans to specific clinical needs rather than defaulting to a 30-day cycle. For example, implement 7-day monitoring for post-surgical recovery or 14-day tracking for lifestyle interventions that align with the 2–15 day billing window. This approach better reflects patient care needs while optimizing the use of the new billing codes.
Expanding RPM Programs for Long-Term Growth
With updated systems and trained staff in place, you can broaden your RPM services to include a wider range of patients. The CPT 99445 code allows billing for patients requiring only 2–15 days of monitoring, such as those transitioning from hospital discharge or undergoing medication adjustments. Similarly, CPT 99470 enables care for low-acuity chronic conditions that need 10–19 minutes of monthly management.
The permanent virtual supervision rule supports scaling operations by enabling distributed clinical teams to work without the constraints of physical proximity. This is especially beneficial for practices managing large patient populations across multiple locations or serving rural areas. Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) can further expand RPM by integrating it with new Advanced Primary Care Management (APCM) behavioral health add-on codes (G0568, G0569, G0570).
Target patient populations previously excluded by the 16-day requirement, such as those needing acute care monitoring, obesity management, or post-procedural recovery. Revise vendor contracts to reflect the updated 10-minute and 2-day billing thresholds, and ensure your platform can automatically distinguish between transmission periods to select the appropriate code.
"These new codes empower providers to engage patients more meaningfully and operate programs that are both clinically effective and financially sustainable." – Dr. Kang, CEO, KangarooHealth
Standardize documentation practices to protect against audit risks. Care teams must record at least one real-time, synchronous interaction per month, as asynchronous communication methods like text messages or voicemails do not qualify. These adjustments not only safeguard compliance but also reinforce the clinical quality of your program. By implementing these changes, practices can develop RPM programs that deliver both high-quality care and sustainable financial outcomes over the long term.
Conclusion: Getting Ready for RPM in 2026
The 2026 CMS updates mark a pivotal shift in how Remote Patient Monitoring (RPM) programs function and generate revenue. With the introduction of CPT 99445 for 2–15 days of monitoring and CPT 99470 for 10–19 minutes of management time, practices now have greater flexibility to provide timely, patient-centered care. These changes eliminate rigid thresholds, opening doors to reimbursements that were previously unattainable.
To thrive under these new guidelines, practices need to make operational adjustments. This includes updating technology systems, training staff, and ensuring precise documentation. For instance, your EHR and RPM platforms should be configured to differentiate between short-duration and standard monitoring while automatically tracking time increments. Additionally, teams must be trained to apply the correct CPT codes and document real-time interactions, as text messages or voicemails alone won’t suffice for compliance.
"For compliant programs, the message is clear: continue to document thoroughly, use technology that enforces payer rules, and partner only with vendors that maintain strict medical-necessity standards." – Daniel Tashnek, JD, Co-founder, Prevounce Health
With the Office of Inspector General increasing its focus on RPM billing, audit readiness is more critical than ever. Practices must maintain detailed logs that include medical necessity documentation, device activity, cumulative time tracking with dates and staff names, and summaries of patient interactions. High-volume RPM clinics billing under their own NPIs face heightened scrutiny, making standardized documentation protocols a non-negotiable necessity. This level of preparedness is key to capitalizing on new revenue streams while avoiding compliance risks.
FAQs
What changes do the new CPT codes 99445 and 99470 bring to RPM billing?
The introduction of CPT 99445 allows healthcare providers to bill for remote patient monitoring (RPM) device supply and daily data transmission when patients send data for 2–15 days during a 30-day period. This code offers reimbursement of approximately $47 but cannot be billed in conjunction with the longer-duration 99454 code.
Additionally, CPT 99470 provides a billing option for 10–19 minutes of RPM treatment management, which must include at least one interactive communication with the patient each month. This service, reimbursed at around $26, replaces the first-20-minute 99457 code.
These updates create more options for billing shorter monitoring periods and managing mid-level RPM services, enabling practices to better tailor their programs to meet both patient needs and Centers for Medicare & Medicaid Services (CMS) guidelines.
What are the new virtual supervision rules for RPM under the 2026 CMS updates?
Starting in 2026, CMS will enforce virtual direct supervision for Remote Patient Monitoring (RPM) services that include treatment-management time. This means a qualified healthcare professional - such as a physician, nurse practitioner, or physician assistant - must be available in real time via interactive communication methods like video or audio during the service. Additionally, this interaction must be carefully documented in the patient’s medical record.
To secure reimbursement for codes like CPT 99470 (first 10 minutes) and CPT 99457 (first 20 minutes), providers must record at least one real-time interaction with the patient or their caregiver within the calendar month. This documentation needs to specify the date, time, method of communication, and the supervising professional’s information. Failing to adhere to these requirements could lead to payment denials or potential audit complications.
How can practices adjust their EHR systems to meet the new RPM billing requirements for 2026?
To prepare for the 2026 CMS updates, practices should adjust their EHR systems to automatically track critical metrics such as patient monitoring days and clinician management minutes, which are essential for meeting the requirements of the new RPM codes. Incorporate streamlined workflows that include CPT codes for device supply and treatment management. Additionally, embed CMS-compliant language directly into encounter note templates to ensure proper documentation.
Leverage the EHR’s billing engine to automatically map thresholds to the appropriate codes. For instance, use CPT 99445 for up to 15 days of monitoring data and CPT 99454 for 16 or more days. Set up alerts to identify gaps in documentation or insufficient management time, and utilize compliance checklists to confirm all requirements are met before submitting claims. Regularly review performance reports to identify discrepancies early, reducing audit risks and optimizing reimbursement under the revised guidelines.
2026 CMS RPM Billing Codes: Requirements and Reimbursement Rates
The Centers for Medicare & Medicaid Services (CMS) has introduced two new CPT codes for 2026, aiming to cover clinical work that previously went uncompensated. These codes - 99445 for device supply and 99470 for treatment management - work in tandem with existing Remote Patient Monitoring (RPM) codes, creating a more adaptable billing framework. The 2026 Medicare conversion factor reflects incremental changes for both non-Advanced Payment Model (APM) and qualifying APM participants.
New and Modified CPT Codes
The new CPT 99445 applies to device supply with data transmission for 2–15 days in a 30-day period, while the existing CPT 99454 continues to require at least 16 days. Similarly, CPT 99470 covers the first 10–19 minutes of treatment management within a calendar month, complementing CPT 99457, which remains applicable for 20 minutes or more. CMS has finalized equal reimbursement for device supply codes - both 99445 and 99454 - at approximately $47, reflecting consistent practice expenses regardless of monitoring duration. For treatment management, CPT 99470 is reimbursed at around $26, roughly half the rate of CPT 99457.
Billing teams must select the single code that aligns with the patient’s actual monitoring or management duration. Additionally, all treatment management codes require at least one real-time interactive communication with the patient or caregiver.
CPT Code | Description | Threshold | 2026 Approx. Rate |
|---|---|---|---|
99445 | 2–15 day device supply | 2–15 days / 30 days | ~$47 |
99454 | 16–30 day device supply | 16–30 days / 30 days | ~$47 |
99470 | Treatment management (first) | 10–19 min / month | ~$26 |
99457 | Treatment management (first) | 20+ min / month | ~$52 |
99458 | Treatment management (add-on) | +20 min increments | ~$41 |
99453 | Initial setup and education | One‑time | ~$22 |
These updates address previous gaps in billing thresholds and introduce more precise time requirements for RPM services.
Reduced Time Requirements for RPM Billing
The updated thresholds resolve a critical issue in RPM reimbursement. Data reveals that 16% of patients recorded 2–15 readings, and 6% received 10–20 minutes of clinical staff time - services that previously went unpaid. These patients, often requiring short-term monitoring for medication adjustments, post-surgical recovery, or acute symptom management, were unable to meet the previous benchmarks of 16 days of monitoring or 20 minutes of clinical management.
"By recognizing shorter monitoring windows and smaller time increments, CMS is rewarding meaningful engagement instead of arbitrary thresholds", remarked Vivo Care.
Practices can now bill for patients who record vitals for as few as two days within a 30-day period or who receive a minimum of 10 minutes of clinical management. However, billing teams must carefully track monitoring days and management minutes, as 99445 and 99454 cannot be billed simultaneously for the same patient in the same month.
Changes to Reimbursement Rates
The revised billing structure for 2026 not only simplifies RPM coding but also enhances revenue opportunities by capturing services that were previously uncompensated. For instance, in June 2025, a clinic in Upstate New York managing 522 patients with hypertension and diabetes identified 83 patients (16%) with 2–15 readings and 31 patients (6%) receiving 10–20 minutes of staff time. Under the 2025 rules, these services generated no revenue. With the 2026 updates, the clinic projects an annual revenue increase of $101,124.
CMS is now using the Hospital Outpatient Prospective Payment System (OPPS) Geometric Mean Cost (GMC) data to establish valuations for technical RPM services like device supply codes. This methodology promotes transparency and ensures more predictable rate-setting. Practices can expect care management revenue to grow by an estimated 10% to 20% under the 2026 guidelines.
Daniel Tashnek, JD, Co-Founder and CEO of Prevounce Health, stated: "The 2026 final rule represents a tangible shift toward that goal, pairing clinical flexibility with improved financial stability."
Key considerations for billing teams:
Update EHR and billing systems to differentiate between 2–15 days (99445) and 16–30 days (99454) of data transmission.
Monitor clinical staff time meticulously to determine whether the 10-minute (99470) or 20-minute (99457) threshold is met in a given month.
Document the date, method, and summary of required real-time interactive communication for all treatment management codes.
Confirm that commercial payers have adjusted their fee schedules to include 99445 and 99470, as Medicare adoption does not guarantee immediate alignment from private insurers.
Documentation and Compliance Requirements
The 2026 CMS updates introduce revised billing thresholds, offering more flexibility but requiring meticulous record-keeping to ensure audit readiness. As billing practices evolve, accurate documentation becomes essential for maximizing RPM revenue. Providers must maintain comprehensive records that capture clinical staff activities and all real-time patient interactions. Following a 2024 report highlighting billing discrepancies, the Office of Inspector General is expected to increase scrutiny of RPM claims through audits.
Documentation Standards for Audits
Four key documentation elements are required to support every RPM claim.
First, providers must clearly establish that remote monitoring is medically necessary for diagnosing or treating a specific illness or injury.
Second, practices must maintain daily logs confirming the digital transmission of physiological data from the patient’s device. For CPT 99445, at least two days of data within a 30-day period must be logged, while CPT 99454 requires a minimum of 16 days. Only digitally gathered data satisfies this requirement.
Third, detailed records must include specific dates, staff identities, and total minutes spent on care activities. This supports the time thresholds of 10–19 minutes (CPT 99470) or 20+ minutes (CPT 99457). While voicemails and asynchronous messages can contribute to total care management time, they do not meet the requirement for interactive communication.
Fourth, synchronous communication must be documented. For CPT codes 99470, 99457, and 99458, providers must record the date, method, and a summary of each real-time, two-way interaction. Text messages, voicemails, manual uploads, or AI-generated conversations do not qualify as interactive communication.
"For compliant programs, the message is clear: continue to document thoroughly, use technology that enforces payer rules, and partner only with vendors that maintain strict medical-necessity standards." – Daniel Tashnek, JD, Co-Founder of Prevounce Health
Meeting these documentation standards ensures practices can align with updated supervision and eligibility requirements.
Eligibility and Supervision Rules
In addition to documentation mandates, CMS has clarified supervision and patient eligibility rules. The agency has permanently adopted a definition of direct supervision that allows "immediate availability" through real-time audio-video technology for incident-to services. This means supervising physicians or advanced practitioners are no longer required to be physically present when clinical staff provide RPM services. However, documentation must demonstrate that the supervising practitioner was accessible via live two-way video, as audio-only communication does not meet the interactive communication standard established for 2026.
This virtual supervision model applies to clinical staff, including third-party RPM vendors, working as an extension of the practice. Supervising clinicians retain the authority to determine whether virtual direct supervision is appropriate for patient safety on a case-by-case basis. These updated supervision standards complement the billing and documentation improvements, ensuring smooth operational workflows.
The 2026 updates also broaden patient eligibility criteria. Beyond chronic conditions, RPM services now include post-operative care, sleep disorders, medication titration, and transitional care after hospital discharge. Practices must document the medical necessity for each episode of care. Additionally, when a patient is discharged and later re-enrolled for a new clinical reason, a new patient consent form must be obtained and documented.
Key compliance considerations:
Configure EHR templates to capture the interactive communication summaries required for the new 10-minute management code CPT 99470.
Ensure virtual supervision is conducted using two-way audio-video technology.
Avoid billing CPT 99470 (10–19 minutes) and CPT 99457 (20+ minutes) for the same patient in the same month.
How CMS Updates Affect Operations and Finances
The 2026 updates from CMS bring significant changes to Remote Patient Monitoring (RPM) workflows, creating opportunities for practices to capture additional revenue. By lowering time and monitoring thresholds, these updates open doors for billing services that were previously excluded, while also requiring operational adjustments to ensure compliance and reduce claim denials. Practices that refine their staffing strategies, enhance documentation systems, and adjust patient selection criteria can expect improvements in both clinical outcomes and financial performance.
Adjusting Workflows for Short-Duration Monitoring
With the introduction of CPT 99445, clinical teams can now integrate short-term monitoring into their care plans. This code allows billing for 2–15 days of data transmission within a 30-day period, making it particularly useful for scenarios such as medication titration, post-surgical recovery, or acute care transitions. For example, a patient adjusting diabetes medication after being discharged from the hospital might require monitoring for only two weeks. Under the new guidelines, this generates $47 in device supply reimbursement, which was previously unbillable due to the stricter 16-day requirement.
Additionally, CPT 99470 enables practices to bill for 10–19 minutes of monthly care coordination, valued at $26. This allows for shorter, more frequent patient interactions, eliminating the need to wait for 20 minutes of cumulative management time. To optimize this process, practices should update their EHR systems to flag when patients reach the 10-minute threshold and ensure all synchronous communications are documented. Virtual supervision further supports distributed clinical teams, enabling seamless operations.
"Clinicians can now bill for fewer monthly vital readings and shorter management time. For patients, this means RPM programs can finally match clinical reality." – Daniel Tashnek, JD, Co-founder, Prevounce Health
These updates not only streamline workflows but also provide new avenues for revenue, as explored below.
Effects on Revenue and Claim Denials
The reduced billing thresholds now make it possible to capture revenue for services that were previously excluded. For instance, practices often lost revenue when patients transmitted data for only 10–15 days or when clinical staff spent just 15 minutes on care coordination. The 2026 updates address these gaps, particularly benefiting patients with lower acuity who need less intensive monitoring but still gain from remote oversight.
However, it’s important to note that billing codes are mutually exclusive within a given month. To avoid claim denials, practices should configure billing systems to automatically select the appropriate code based on actual patient engagement data. Although these changes offer greater flexibility, the Office of Inspector General (OIG) continues to closely monitor RPM claims for medical necessity and proper documentation of interactive communication. Regular internal audits are essential to maintain compliance and minimize denials.
2025 Requirement | 2026 New Option | Revenue Impact |
|---|---|---|
Minimum 16 days of data | 2–15 days of data (CPT 99445) | Captures $47 for short-term episodes |
Minimum 20 minutes management | 10–19 minutes management (CPT 99470) | Captures $26 for low-acuity check-ins |
Physical direct supervision | Permanent virtual supervision | Reduces overhead for clinical staff oversight |
These updates not only provide financial benefits but also expand the scope of RPM services to reach more patients.
Serving More Patient Populations
The new CMS guidelines allow practices to extend RPM services to a broader range of patient needs. Beyond chronic conditions, practices can now bill for post-operative care, sleep disorders, medication titration, and transitional care following hospital discharge. This shift toward episodic monitoring reflects real-world clinical scenarios, where patients often need intensive monitoring during specific treatment phases rather than continuous oversight.
Practices should review their patient panels to identify individuals who were previously ineligible for RPM services but now qualify under the updated thresholds. For example, a patient recovering from joint replacement surgery may need only short-term monitoring, which qualifies for CPT 99445 and CPT 99470. Each enrollment must include documented medical necessity for the specific condition being treated. Additionally, if a patient is discharged and later re-enrolled for a different clinical issue, a new consent form is required.
"These new codes empower providers to engage patients more meaningfully and operate programs that are both clinically effective and financially sustainable." – Dr. Kang, CEO, KangarooHealth
Key operational considerations include:
Updating EHR templates to track 2–15 day monitoring windows and 10-minute management increments
Training billing staff on mutually exclusive code pairings to avoid denials
Establishing virtual supervision protocols using real-time audio-video technology
Designing specific clinical pathways for short-term monitoring during medication adjustments and post-discharge recovery
Conducting monthly internal audits to ensure proper documentation of medical necessity for all active enrollments
How to Implement the 2026 RPM Updates
Implementing the 2026 updates to Remote Patient Monitoring (RPM) involves three key steps: auditing your current program, training your team, and expanding services.
Reviewing Your Current RPM Program
Start with a detailed audit of your existing RPM platform to ensure it can handle the updated billing thresholds. The system must differentiate between patients transmitting data for 2–15 days versus 16 or more days, as well as track clinical staff time spent on care coordination - 10–19 minutes versus 20+ minutes. Without these capabilities, you risk billing errors, missed opportunities for reimbursement, or claim denials.
Next, identify patients who now qualify under the updated CPT 99445 and CPT 99470 codes. These include individuals needing short-term medication adjustments, those recently discharged from the hospital, or patients requiring episodic monitoring for acute conditions. These new eligibility criteria open doors to services that were previously unavailable.
Ensure your billing systems are equipped to enforce the mutually exclusive code rules introduced in the updates. Additionally, confirm that your supervision model supports the permanent virtual direct supervision rule. This change allows supervising physicians to meet the "immediately available" requirement through real-time audio-video communication, eliminating the need for physical presence.
Finally, stay informed about payer adoption timelines. While Medicare has finalized these codes for 2026, commercial insurers may implement them on varying schedules. Track which payers in your area have approved coverage for CPT 99445 and CPT 99470 to avoid submitting claims that could be rejected.
Once these audits are complete, the focus shifts to updating electronic health record (EHR) systems and training your staff to integrate the new guidelines effectively.
Staff Training and EHR System Updates
Update your EHR and billing systems to incorporate CPT 99445, which covers 2–15 days of data transmission, and CPT 99470, which applies to 10–19 minutes of care management time. Automate time tracking for patient interactions within this 10–19 minute range to ensure accurate billing and reimbursement.
Train clinical teams on the requirements for virtual direct supervision, proper coding, and real-time documentation. The 2026 rule allowing "direct supervision" through real-time audio-video technology enhances team flexibility and efficiency, especially for distributed care teams. However, adhering to documentation and communication protocols is crucial for compliance.
"The interactive communication contributes to the total time, but it does not need to represent the entire cumulative reported time of the treatment management service." – CMS Final Rule
Highlight the importance of "live, interactive communication" for treatment management codes. Staff must conduct at least one real-time phone or video interaction per month to bill for CPT 99470, 99457, or 99458; text messages or voicemails alone do not meet the requirements. Update EHR templates to include logs for timing and communication, ensuring records are audit-ready, as RPM billing continues to face scrutiny from the Office of Inspector General (OIG).
Tailor monitoring plans to specific clinical needs rather than defaulting to a 30-day cycle. For example, implement 7-day monitoring for post-surgical recovery or 14-day tracking for lifestyle interventions that align with the 2–15 day billing window. This approach better reflects patient care needs while optimizing the use of the new billing codes.
Expanding RPM Programs for Long-Term Growth
With updated systems and trained staff in place, you can broaden your RPM services to include a wider range of patients. The CPT 99445 code allows billing for patients requiring only 2–15 days of monitoring, such as those transitioning from hospital discharge or undergoing medication adjustments. Similarly, CPT 99470 enables care for low-acuity chronic conditions that need 10–19 minutes of monthly management.
The permanent virtual supervision rule supports scaling operations by enabling distributed clinical teams to work without the constraints of physical proximity. This is especially beneficial for practices managing large patient populations across multiple locations or serving rural areas. Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) can further expand RPM by integrating it with new Advanced Primary Care Management (APCM) behavioral health add-on codes (G0568, G0569, G0570).
Target patient populations previously excluded by the 16-day requirement, such as those needing acute care monitoring, obesity management, or post-procedural recovery. Revise vendor contracts to reflect the updated 10-minute and 2-day billing thresholds, and ensure your platform can automatically distinguish between transmission periods to select the appropriate code.
"These new codes empower providers to engage patients more meaningfully and operate programs that are both clinically effective and financially sustainable." – Dr. Kang, CEO, KangarooHealth
Standardize documentation practices to protect against audit risks. Care teams must record at least one real-time, synchronous interaction per month, as asynchronous communication methods like text messages or voicemails do not qualify. These adjustments not only safeguard compliance but also reinforce the clinical quality of your program. By implementing these changes, practices can develop RPM programs that deliver both high-quality care and sustainable financial outcomes over the long term.
Conclusion: Getting Ready for RPM in 2026
The 2026 CMS updates mark a pivotal shift in how Remote Patient Monitoring (RPM) programs function and generate revenue. With the introduction of CPT 99445 for 2–15 days of monitoring and CPT 99470 for 10–19 minutes of management time, practices now have greater flexibility to provide timely, patient-centered care. These changes eliminate rigid thresholds, opening doors to reimbursements that were previously unattainable.
To thrive under these new guidelines, practices need to make operational adjustments. This includes updating technology systems, training staff, and ensuring precise documentation. For instance, your EHR and RPM platforms should be configured to differentiate between short-duration and standard monitoring while automatically tracking time increments. Additionally, teams must be trained to apply the correct CPT codes and document real-time interactions, as text messages or voicemails alone won’t suffice for compliance.
"For compliant programs, the message is clear: continue to document thoroughly, use technology that enforces payer rules, and partner only with vendors that maintain strict medical-necessity standards." – Daniel Tashnek, JD, Co-founder, Prevounce Health
With the Office of Inspector General increasing its focus on RPM billing, audit readiness is more critical than ever. Practices must maintain detailed logs that include medical necessity documentation, device activity, cumulative time tracking with dates and staff names, and summaries of patient interactions. High-volume RPM clinics billing under their own NPIs face heightened scrutiny, making standardized documentation protocols a non-negotiable necessity. This level of preparedness is key to capitalizing on new revenue streams while avoiding compliance risks.
FAQs
What changes do the new CPT codes 99445 and 99470 bring to RPM billing?
The introduction of CPT 99445 allows healthcare providers to bill for remote patient monitoring (RPM) device supply and daily data transmission when patients send data for 2–15 days during a 30-day period. This code offers reimbursement of approximately $47 but cannot be billed in conjunction with the longer-duration 99454 code.
Additionally, CPT 99470 provides a billing option for 10–19 minutes of RPM treatment management, which must include at least one interactive communication with the patient each month. This service, reimbursed at around $26, replaces the first-20-minute 99457 code.
These updates create more options for billing shorter monitoring periods and managing mid-level RPM services, enabling practices to better tailor their programs to meet both patient needs and Centers for Medicare & Medicaid Services (CMS) guidelines.
What are the new virtual supervision rules for RPM under the 2026 CMS updates?
Starting in 2026, CMS will enforce virtual direct supervision for Remote Patient Monitoring (RPM) services that include treatment-management time. This means a qualified healthcare professional - such as a physician, nurse practitioner, or physician assistant - must be available in real time via interactive communication methods like video or audio during the service. Additionally, this interaction must be carefully documented in the patient’s medical record.
To secure reimbursement for codes like CPT 99470 (first 10 minutes) and CPT 99457 (first 20 minutes), providers must record at least one real-time interaction with the patient or their caregiver within the calendar month. This documentation needs to specify the date, time, method of communication, and the supervising professional’s information. Failing to adhere to these requirements could lead to payment denials or potential audit complications.
How can practices adjust their EHR systems to meet the new RPM billing requirements for 2026?
To prepare for the 2026 CMS updates, practices should adjust their EHR systems to automatically track critical metrics such as patient monitoring days and clinician management minutes, which are essential for meeting the requirements of the new RPM codes. Incorporate streamlined workflows that include CPT codes for device supply and treatment management. Additionally, embed CMS-compliant language directly into encounter note templates to ensure proper documentation.
Leverage the EHR’s billing engine to automatically map thresholds to the appropriate codes. For instance, use CPT 99445 for up to 15 days of monitoring data and CPT 99454 for 16 or more days. Set up alerts to identify gaps in documentation or insufficient management time, and utilize compliance checklists to confirm all requirements are met before submitting claims. Regularly review performance reports to identify discrepancies early, reducing audit risks and optimizing reimbursement under the revised guidelines.

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Dec 28, 2025
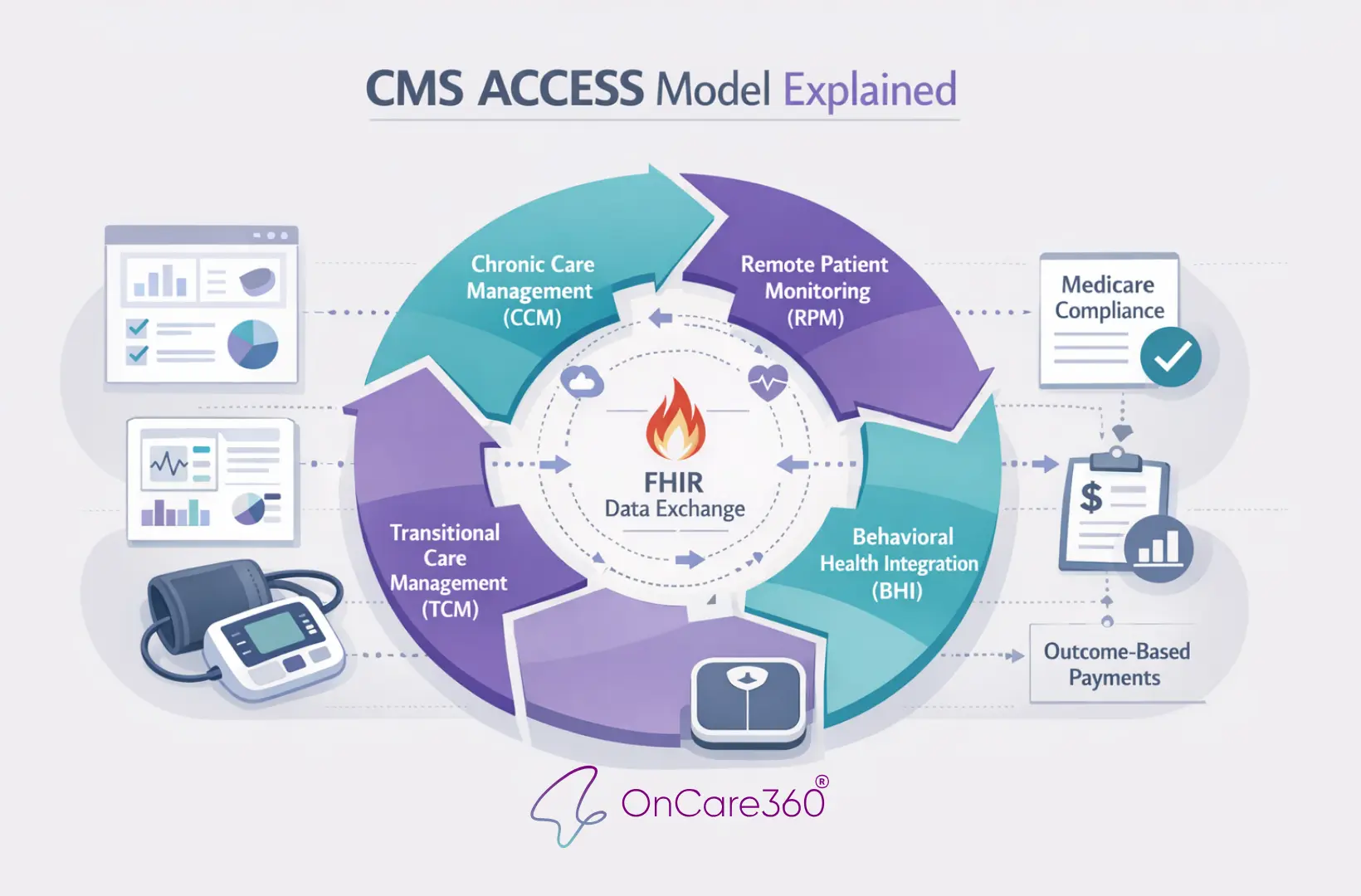
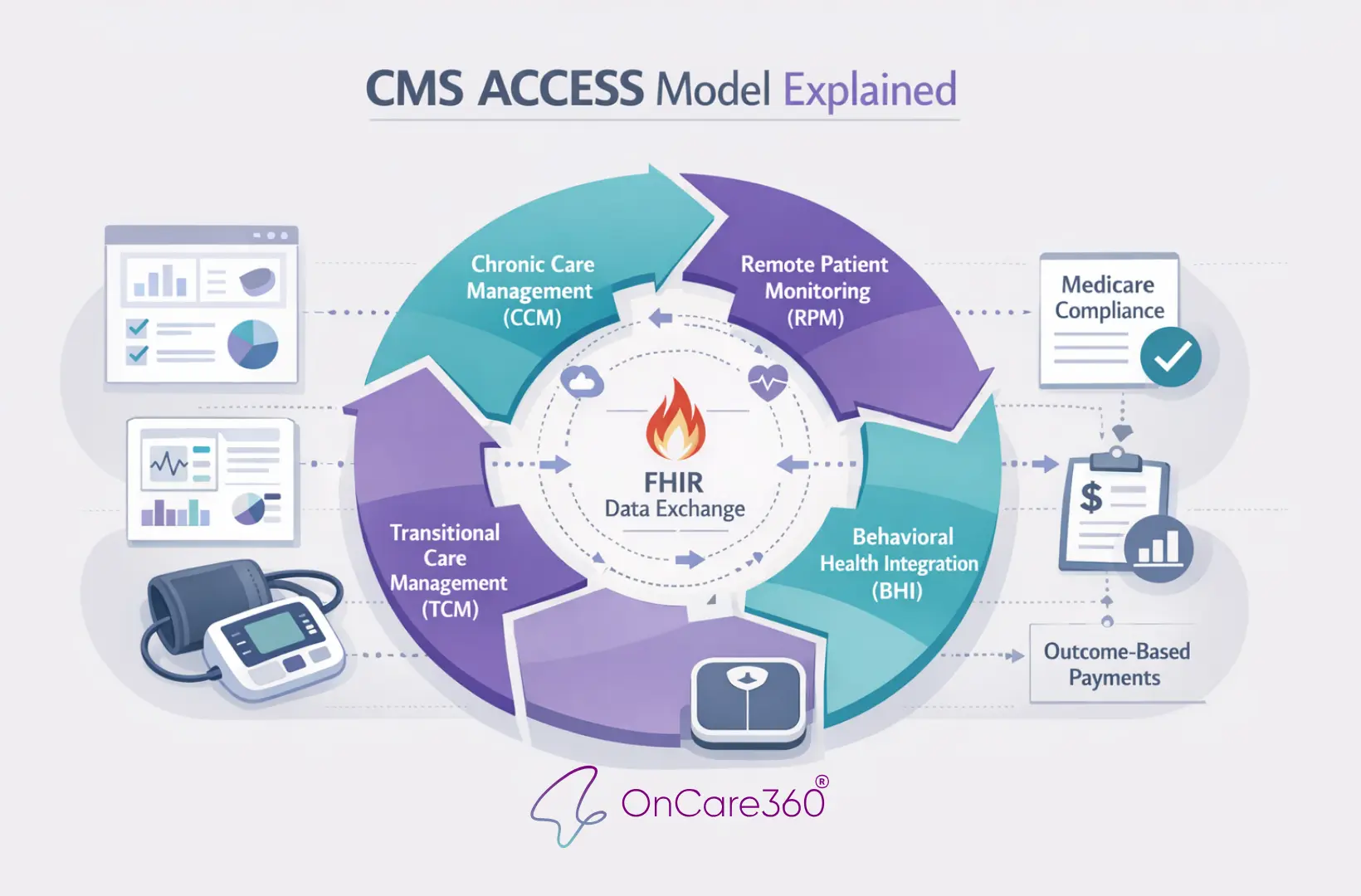
CMS ACCESS Model Explained

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Dec 28, 2025
CMS ACCESS Model Explained
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?


