CMS ACCESS Model Explained
OnCare360
Dec 28, 2025
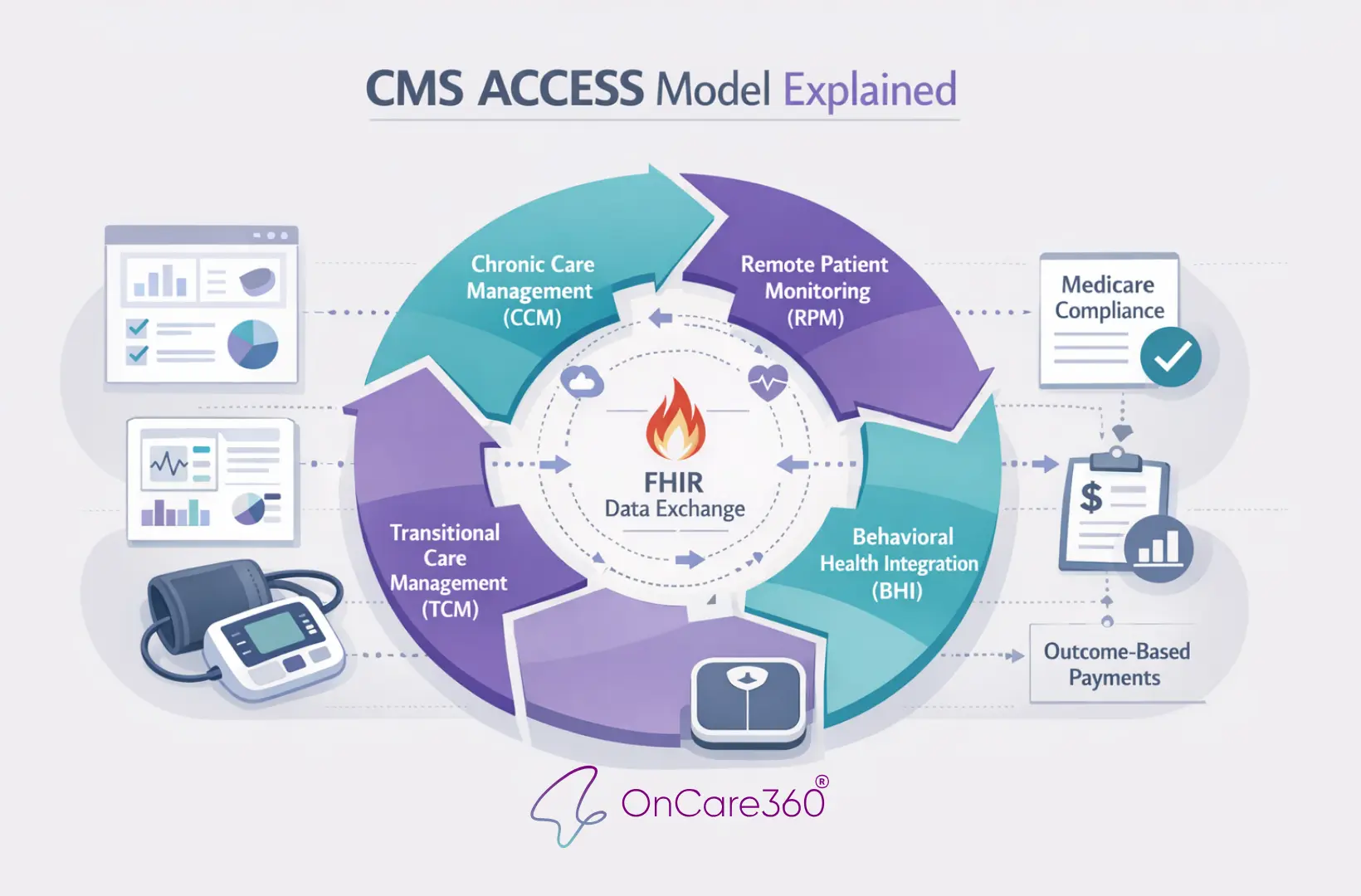
The CMS ACCESS Model is a new Medicare initiative launching on July 5, 2026, designed to improve chronic disease management through Outcome-Aligned Payments (OAPs). Unlike traditional fee-for-service systems, ACCESS ties payments directly to measurable health outcomes, such as improved blood pressure or reduced depression symptoms. This model targets four key areas - cardio-kidney-metabolic risk, musculoskeletal pain, behavioral health, and established chronic diseases - impacting over two-thirds of Medicare beneficiaries.
For physician groups, practice administrators, and value-based care leaders, ACCESS offers a streamlined approach to care delivery by focusing on technology-enabled monitoring, direct patient enrollment, and outcome-based reimbursements. This article outlines the model’s clinical tracks, eligibility requirements, and payment structures, offering actionable insights for organizations preparing to participate.
Eligibility and Operational Requirements
Joining the ACCESS Model involves meeting specific enrollment criteria and maintaining the necessary systems to support outcome-based care. To qualify, organizations must be Medicare Part B-enrolled providers with the infrastructure to monitor clinical outcomes, electronically coordinate care with other providers, and adhere to federal privacy and safety standards. Below, we outline the eligibility requirements and operational obligations for participation.
Who Can Participate
The cornerstone of ACCESS eligibility is Medicare Part B enrollment. Organizations must be active providers or suppliers with a valid TIN and NPI. Those not yet enrolled must complete the process through the Provider Enrollment, Chain, and Ownership System (PECOS) before their ACCESS application can be approved by CMS.
Certain provider categories are excluded from participation. For instance, Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) suppliers, as well as laboratory suppliers, are ineligible. Technology companies that are not enrolled in Medicare Part B have two options: they can either enroll directly or partner with an enrolled provider who will act as the official ACCESS participant.
Each participating organization is required to appoint a physician Clinical Director (or Medical Director) who is Medicare-enrolled. This individual is responsible for ensuring oversight, maintaining quality standards, and meeting regulatory requirements. This role underscores the importance of physician-led accountability, even when day-to-day operations involve nurses, health coaches, or digital tools.
Participants must also meet state licensure requirements, operate as HIPAA-covered entities, and ensure that their devices and software comply with FDA regulations. Exceptions may apply under programs like the TEMPO pilot, which allows for FDA enforcement discretion. For organizations relying on digital health tools, verifying regulatory status early is essential, as FDA compliance can impact the timeline for application approval.
Required Infrastructure and Capabilities
Beyond eligibility, participants must establish a strong technical foundation. The ACCESS Model requires infrastructure built around FHIR-based data interoperability. Participants must use CMS-hosted, standards-based APIs for eligibility checks, patient enrollment, and reporting clinical outcome measures. Your EHR or care management platform must be capable of exchanging structured data using modern standards.
Health Information Exchange (HIE) connectivity is another key requirement. Organizations must connect with an HIE or a similar trusted network, such as CMS Aligned Networks, to share electronic care plans and clinical updates with referring primary care providers. Updates must be securely transmitted at key points - such as the start of treatment, its completion, and at defined clinical milestones - using secure methods like Direct messaging. This ensures that primary care providers remain informed, even when care is delivered by specialty providers or through technology-enabled platforms.
The infrastructure must also support longitudinal outcome tracking. Systems need to collect and monitor baseline data and track improvements over time. This could include metrics like blood pressure levels, HbA1c readings, or validated Patient-Reported Outcome Measures (PROMs) for conditions such as pain or behavioral health. Since this data is gathered continuously - not just during office visits - many participants rely on tools like remote monitoring devices, mobile apps, or telehealth platforms to meet the model’s requirements.
Requirement Category | Specific Criteria |
|---|---|
Provider Type | Medicare Part B-enrolled providers/suppliers (excluding DME and labs) |
Leadership | Designated physician Clinical Director (Medicare-enrolled) |
Data Standards | FHIR-based APIs for reporting; HIE connectivity for care coordination |
Privacy/Safety | HIPAA-covered entity status; FDA compliance for devices/software |
Operational | Active TIN; NPI; electronic care plan sharing |
Organizations interested in participating should prioritize completing Medicare enrollment (if not already done), establishing HIE connectivity, and ensuring their digital tools meet FDA compliance standards. CMS will accept applications on a rolling basis from January 2026 through 2033, providing multiple opportunities for entry. However, technical readiness will determine how quickly participants can begin earning Outcome-Aligned Payments.
4 Clinical Tracks in the CMS ACCESS Model
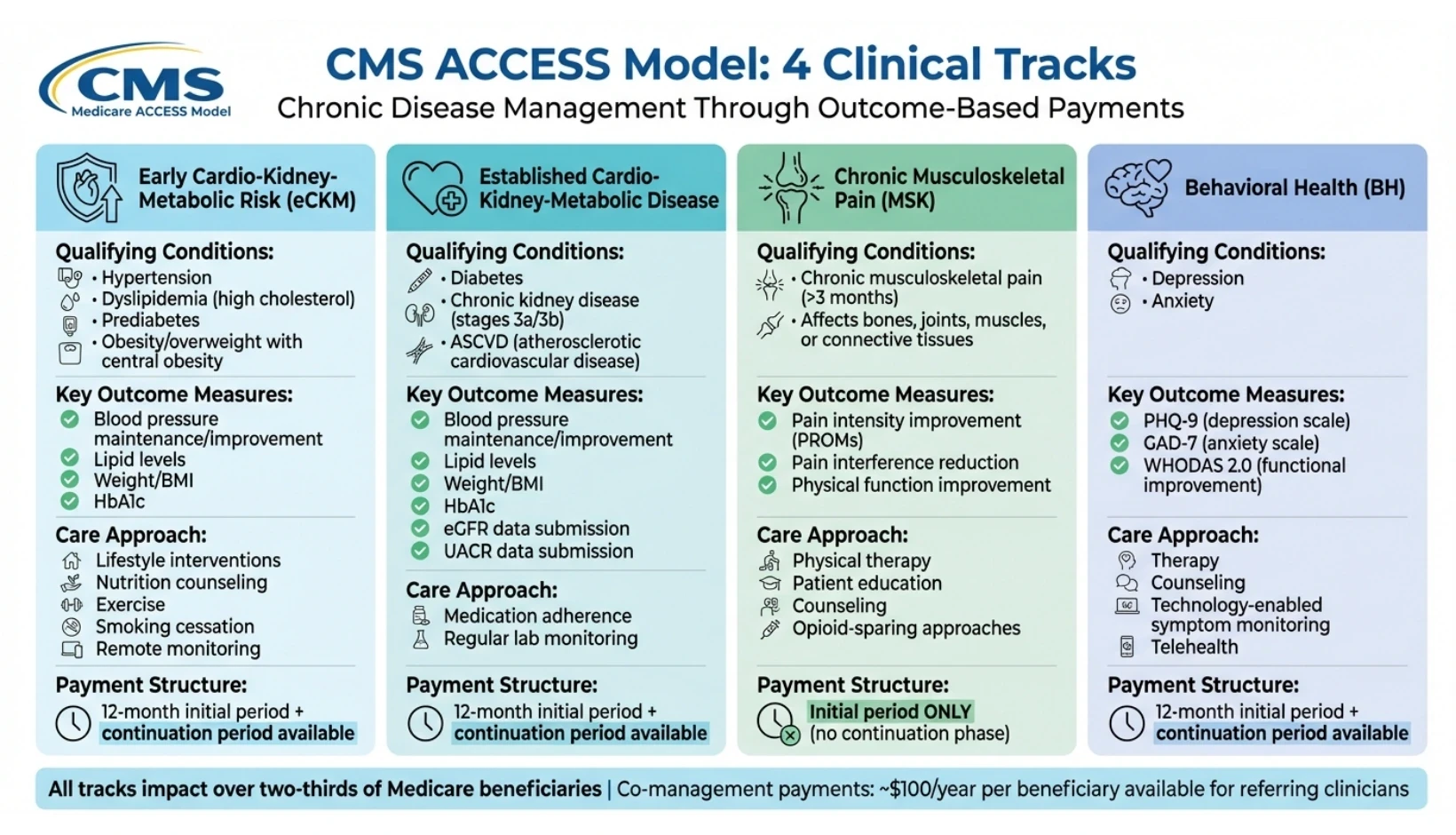
CMS ACCESS Model: 4 Clinical Tracks Comparison Chart
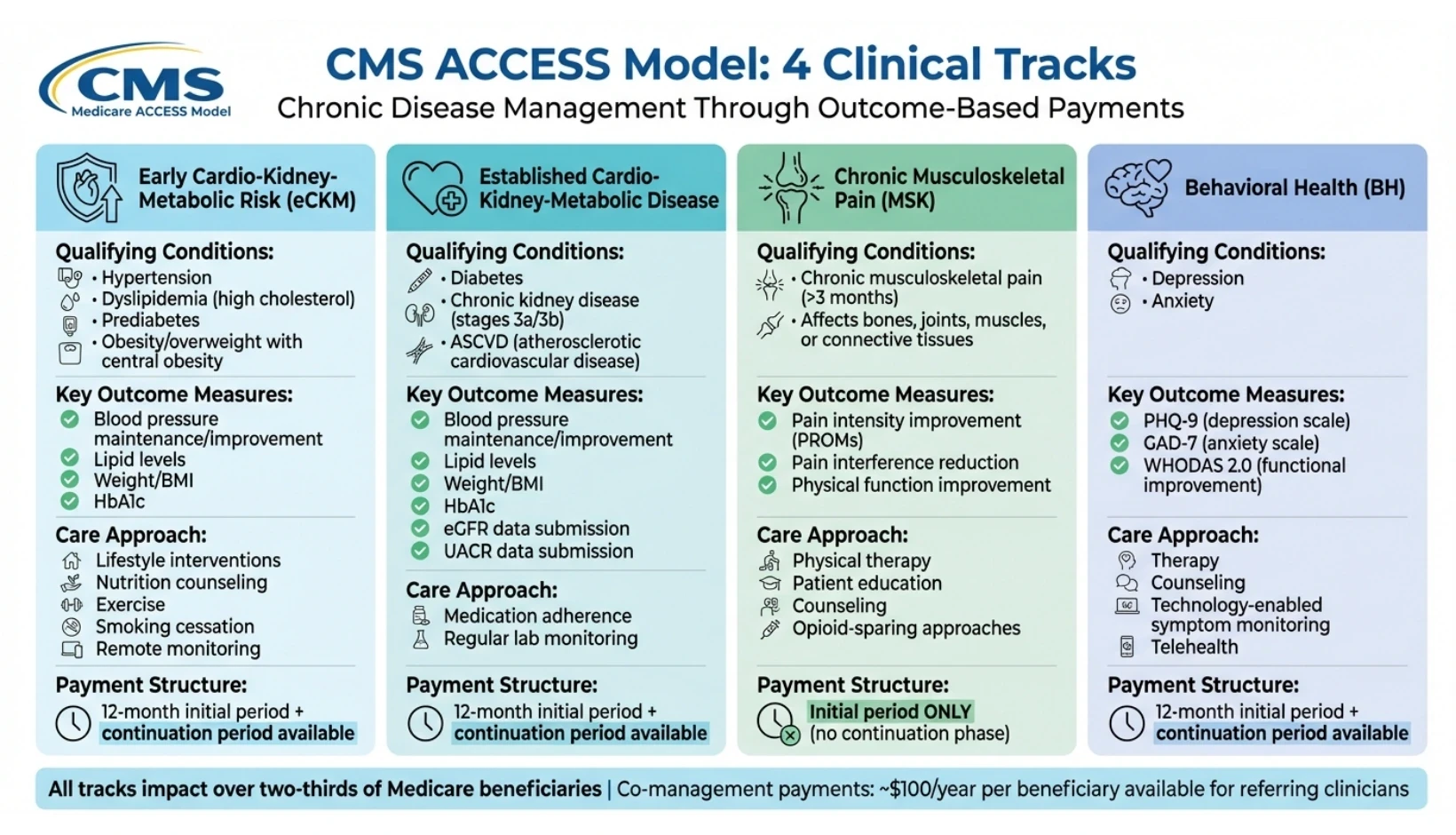
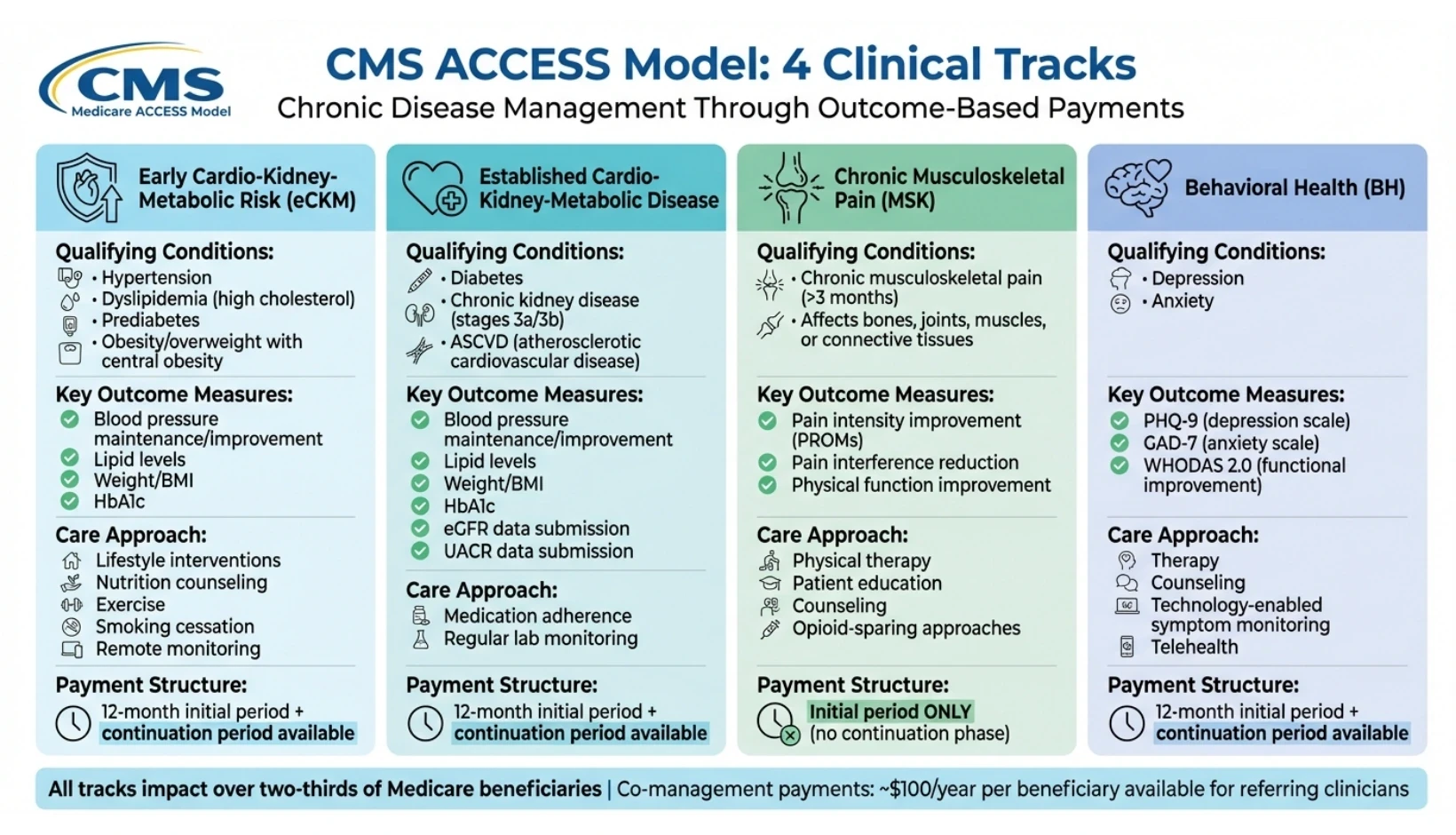
The CMS ACCESS Model organizes care into four distinct clinical tracks, each designed to address chronic conditions that impact over two-thirds of individuals enrolled in Original Medicare. These tracks require providers to manage all qualifying conditions within a given category, ensuring a coordinated, patient-centered approach. Payments are linked to measurable health improvements from each patient's baseline, making accurate and consistent outcome tracking a fundamental requirement. Below is an overview of the clinical tracks, their target conditions, and the associated goals.
Early Cardio-Kidney-Metabolic Risk Track
This track emphasizes early detection and risk management, aiming to intervene before chronic diseases fully develop. It focuses on conditions such as hypertension, dyslipidemia (high cholesterol), prediabetes, and obesity or overweight with signs of central obesity. The approach includes lifestyle interventions such as nutrition counseling, exercise guidance, smoking cessation, and remote monitoring through devices that track blood pressure and weight.
Key outcome measures include maintaining or improving clinical biomarkers like blood pressure, lipid levels, weight (or BMI), and hemoglobin A1c (HbA1c). Providers must establish baseline metrics and demonstrate measurable improvements or stability over time. This track is particularly well-suited for organizations with established wellness and preventive care programs. For more insights on optimizing these initiatives, visit our learning center.
Established Cardio-Kidney-Metabolic Disease Track
Building on the early risk management track, this category addresses patients with more advanced chronic conditions, including diabetes, chronic kidney disease (stages 3a and 3b), and atherosclerotic cardiovascular disease (ASCVD). The focus is on managing these conditions through medication adherence and regular monitoring of lab values.
Outcome measures are similar to the Early CKM Track - improvements in blood pressure, lipid levels, weight, and HbA1c - but with additional requirements. Providers must also submit detailed data on estimated glomerular filtration rate (eGFR) and urine albumin-creatinine ratio (UACR) for patients with chronic kidney disease or diabetes. This added layer of data collection underscores the need for detailed clinical oversight and a structured care approach.
Chronic Musculoskeletal Pain Track
This track targets chronic musculoskeletal pain lasting longer than three months, which can affect bones, joints, muscles, or connective tissues. Treatment strategies include physical therapy, patient education, counseling, and opioid-sparing approaches. Unlike the metabolic tracks, this track relies entirely on Patient Reported Outcome Measures (PROMs) to evaluate success.
Outcome measures focus on improvements in pain intensity, the impact of pain on daily activities, and overall physical function. Providers are expected to achieve meaningful improvements within the initial treatment period, as this track does not include a follow-up continuation phase. It is particularly suited for organizations with strong rehabilitation and pain management programs.
Behavioral Health Conditions Track
This track is designed to manage depression and anxiety through technology-enabled symptom monitoring and treatment adherence. Care delivery includes therapy, counseling, and the use of standardized tools to track symptoms over time.
Outcome measures are based on validated scales, including the Patient Health Questionnaire (PHQ-9) for depression and the Generalized Anxiety Disorder scale (GAD-7) for anxiety. Additionally, providers must submit data from the WHODAS 2.0 12-item scale to assess overall functional improvement. Given the episodic nature of behavioral health issues, this track requires robust systems for telehealth, secure communication, and asynchronous monitoring to ensure consistent patient engagement and progress tracking.
Clinical Track | Qualifying Conditions | Key Outcome Measures |
|---|---|---|
Early CKM (eCKM) | Hypertension, dyslipidemia, prediabetes, obesity/overweight | Maintenance or improvement in BP, lipids, weight/BMI, and HbA1c |
Established CKM | Diabetes, CKD (3a/3b), ASCVD (heart disease) | Maintenance/improvement in BP, lipids, weight, HbA1c; submission of eGFR and UACR data |
Musculoskeletal (MSK) | Chronic musculoskeletal pain (>3 months) | Improvements in pain intensity, interference, and physical function via PROMs |
Behavioral Health (BH) | Depression, anxiety | Symptom improvement (PHQ-9, GAD-7) and functional gains (WHODAS 2.0) |
How Outcome-Aligned Payments Work
The ACCESS Model introduces a new approach called Outcome-Aligned Payments (OAPs), which ties recurring payments to measurable clinical outcomes. To receive full payment, providers must meet specific clinical targets for a significant portion of their enrolled patients. Unlike the traditional fee-for-service system that rewards individual patient successes, the Centers for Medicare & Medicaid Services (CMS) bases these payments on the percentage of patients achieving their outcome goals, with minimum thresholds that increase each year of participation. This payment structure is designed to support ongoing care by enabling continuous monitoring and interventions between office visits.
"By rewarding outcomes rather than defined activities (or volume of services delivered), ACCESS gives clinicians greater flexibility to deliver modern technology-supported care in ways that best improve patient health." - CMS
Most tracks under the model include an initial 12-month care period with higher payment rates. After that, providers can opt for a continuation period at a reduced rate, reflecting the lower resource needs once care is established. For patients enrolled in multiple tracks with the same provider, CMS applies a discount to the total payment to account for administrative efficiencies. The Musculoskeletal (MSK) track, which focuses on addressing chronic pain, is an exception - it offers only the initial care period and no continuation phase. This framework highlights how payment tiers and performance thresholds create financial incentives while maintaining a focus on patient outcomes.
Payment Tiers and Performance Thresholds
The model structures payment tiers around performance thresholds, which represent the minimum percentage of enrolled patients who must meet their clinical targets for providers to receive full payment. These thresholds increase annually to encourage ongoing improvement and engagement. The focus is on measurable progress from each patient's baseline. For instance, a patient with severe hypertension who lowers their systolic blood pressure by 10 mmHg contributes to the threshold, even if their blood pressure hasn’t yet reached the ideal range.
Co-Management Payments
Beyond outcome-aligned payments, the ACCESS Model includes co-management payments for primary care or referring clinicians who collaborate with ACCESS organizations. These payments are approximately $30 for each documented review, with an additional $10 onboarding payment available the first time a clinician helps set up a beneficiary. Clinicians can bill for co-management once every four months per beneficiary, with payments totaling around $100 per beneficiary annually. To qualify, clinicians must review the ACCESS Care Update and document at least one care coordination action in the electronic health record - such as updating a problem list, making a medication change, initiating new monitoring instructions, or providing a referral. There is no cost-sharing for beneficiaries, and advance consent is not required. Starting in 2028, ACCESS payments will be included in ACO REACH and Medicare Shared Savings Program benchmark calculations, but for 2026 and 2027, these payments will not impact ACO benchmarks.
Payment Comparison by Track
Although CMS has not yet provided specific base OAP dollar amounts by track as of December 2025, the payment structure varies depending on the complexity and duration of care. Below is an overview of the general framework:
Track | Initial Care Period | Continuation Period | Co-Management | Key Payment Considerations |
|---|---|---|---|---|
Early CKM (eCKM) | 12 months at full rate | Available at reduced rate | $100/year | Focus on prevention; lower clinical complexity |
Established CKM | 12 months at full rate | Available at reduced rate | $100/year | Higher clinical complexity; requires eGFR/UACR data submission |
Musculoskeletal (MSK) | Initial period only | Not available | $100/year | Designed for pain resolution; no long-term continuation |
Behavioral Health (BH) | 12 months at full rate | Available at reduced rate | $100/year | Episodic care; requires telehealth and remote monitoring |
For rural patients enrolled in qualifying tracks, a fixed adjustment is applied to encourage access in underserved areas. Additionally, participants can choose to waive beneficiary cost-sharing for OAPs to promote engagement.
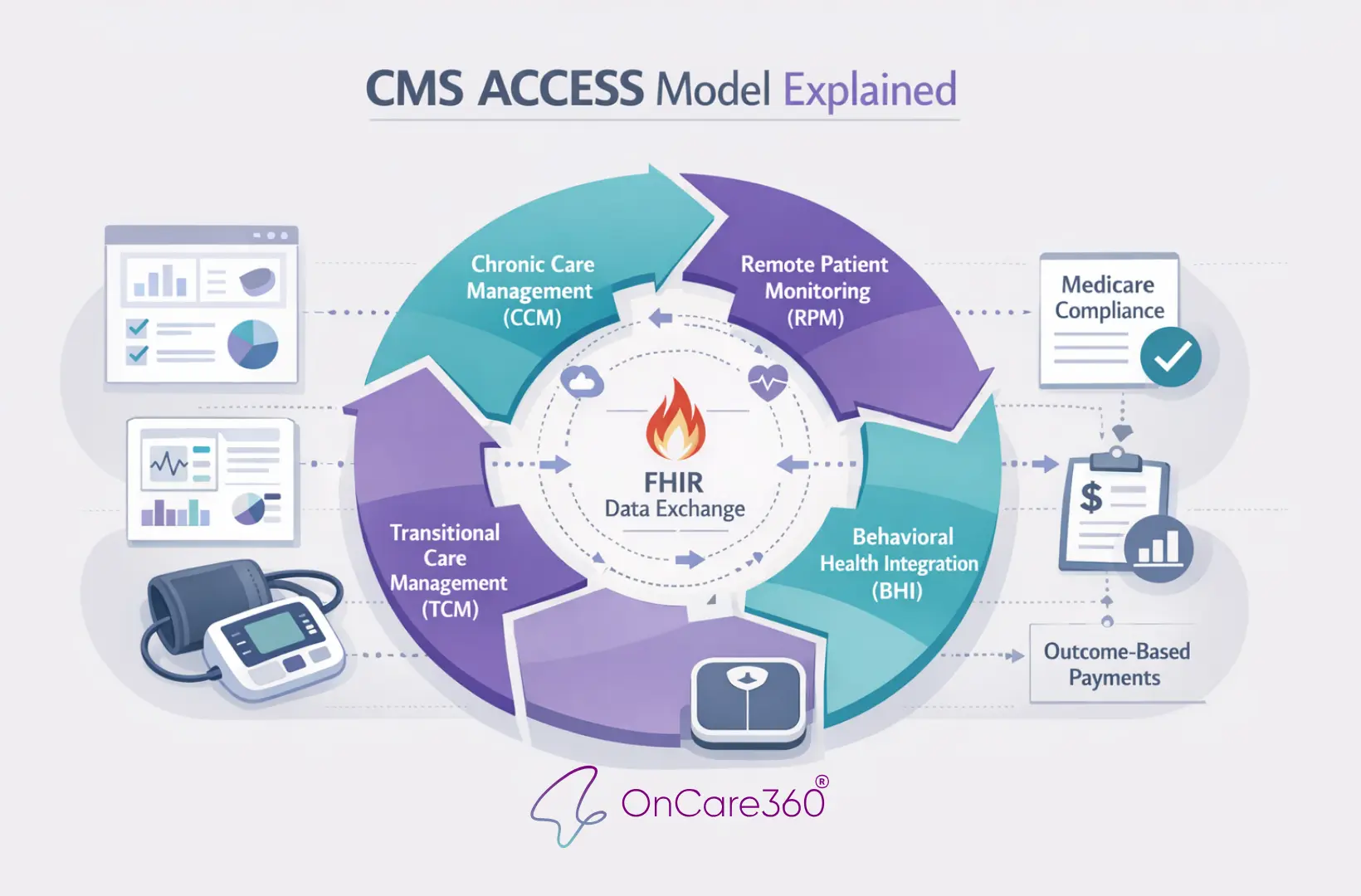
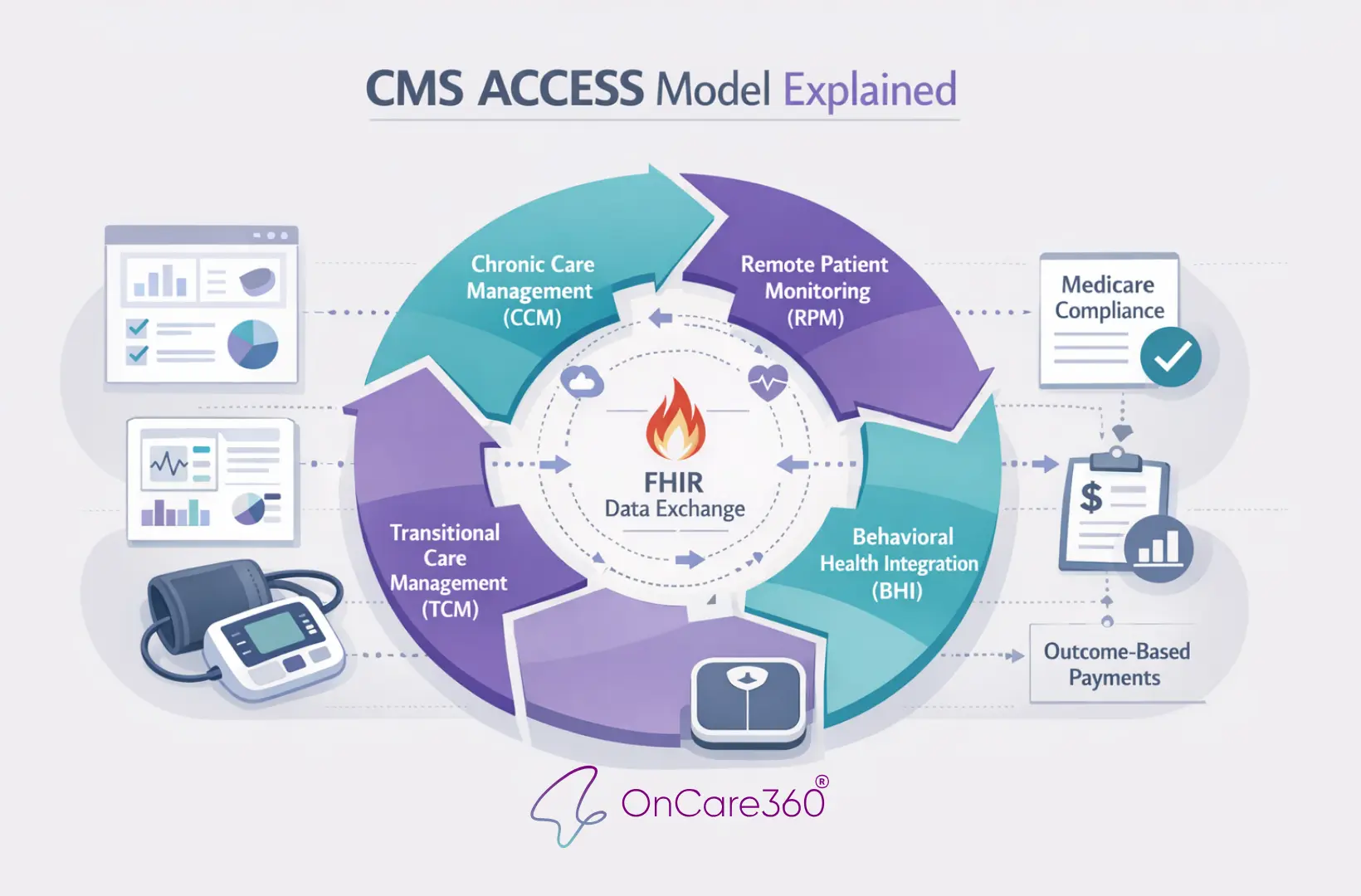
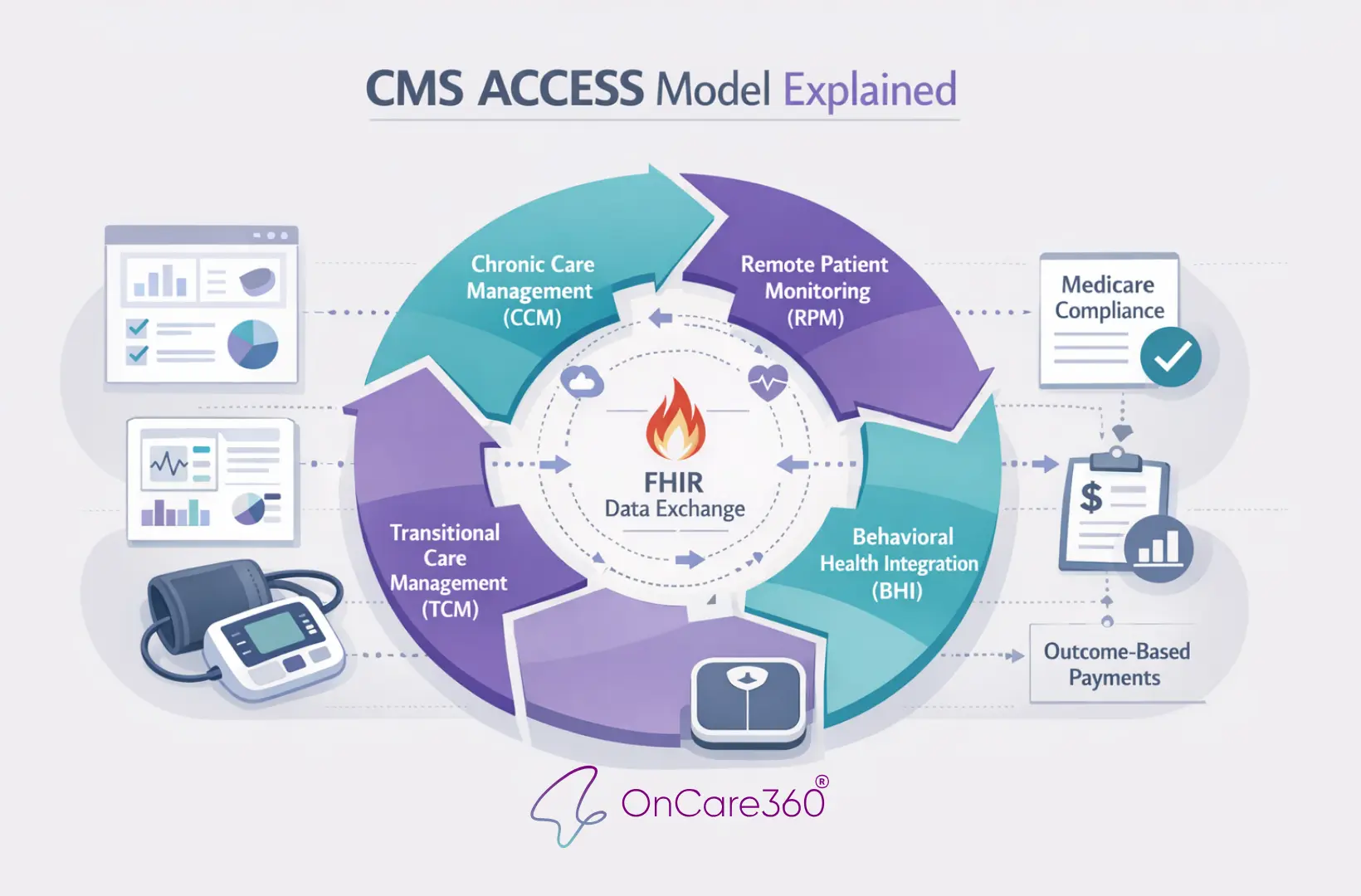
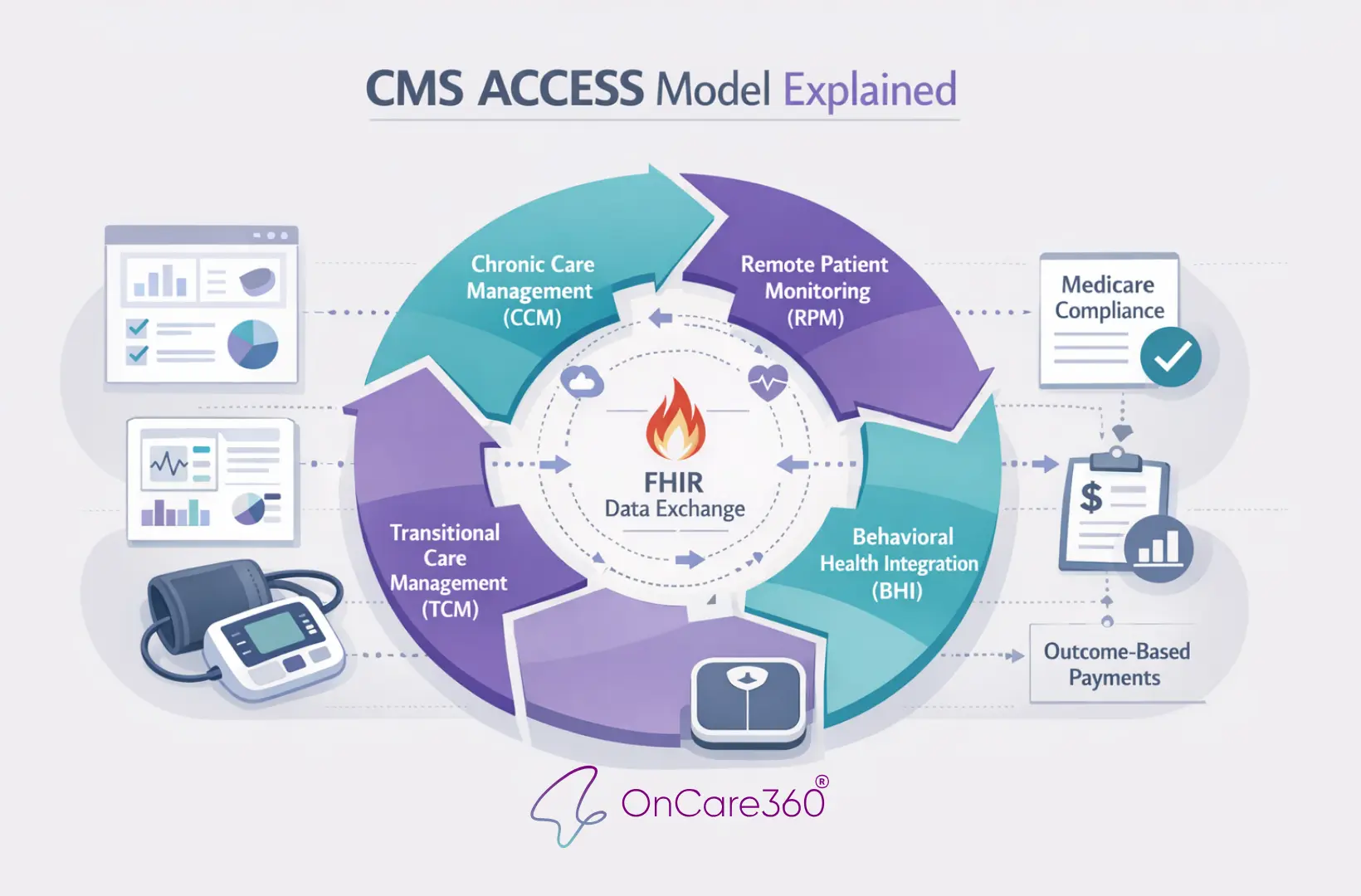
Implementing the CMS ACCESS Model with OnCare360
OnCare360 aligns seamlessly with the CMS ACCESS performance framework, offering a comprehensive solution to integrate care delivery, compliance, and ROI measurement for value-based care initiatives. The platform provides the necessary infrastructure to meet CMS ACCESS operational and compliance standards while scaling between-visit care. By consolidating outcome tracking, API-based reporting, care coordination workflows, and audit-ready documentation, OnCare360 supports all four ACCESS clinical tracks - Early CKM, Established CKM, Musculoskeletal Pain, and Behavioral Health - without requiring separate workflows for each program.
How OnCare360 Supports CMS ACCESS Requirements
OnCare360 simplifies compliance with CMS standards through features like integrated data exchange and preloaded compliance checks, ensuring adherence to API and HIPAA requirements while reducing manual documentation efforts. Real-time dashboards provide Clinical Directors with oversight of patient outcomes, intervention timelines, and progress against annual performance thresholds outlined by the ACCESS Model. The platform also systematically gathers baseline clinical measures - such as HbA1c, blood pressure, and weight - and validated Patient-Reported Outcome Measures (PROMs) like PHQ-9 for depression and GAD-7 for anxiety, which are essential for tracking improvements from each patient’s starting point.
For co-management billing, OnCare360 automates the distribution of ACCESS Care Updates to referring clinicians at key stages: treatment initiation, completion, and clinical milestones. These updates enable primary care providers to document care coordination actions, such as updating problem lists, adjusting treatment plans, or initiating new monitoring protocols. This documentation supports billing of the $30 co-management payment (plus a $10 onboarding modifier for first-time setups) every four months per beneficiary. Secure, automated workflows ensure compliance with CMS interoperability requirements while minimizing administrative workload.
Beyond compliance, OnCare360 enhances care delivery, making it easier to manage high-risk patient populations effectively.
Scaling Between-Visit Care with OnCare360
Once CMS requirements are met, OnCare360’s scalable tools enable care teams to efficiently manage chronic conditions, which impact nearly two-thirds of Medicare beneficiaries. By leveraging AI-driven care coordination, the platform identifies prioritization cues, risk alerts, and documentation suggestions, while licensed clinicians make final care decisions and interventions. This collaborative approach allows smaller care teams to oversee large patient panels without compromising quality.
The platform’s medical-grade cellular devices eliminate setup hurdles by automatically transmitting critical health data - such as blood pressure, glucose, weight, and pulse oximetry - directly to the care platform. These devices don’t require patient Wi-Fi or app downloads, ensuring continuous data flow. This real-time visibility aligns with the ACCESS Model’s focus on between-visit care, enabling timely interventions when clinical metrics deviate from target ranges.
OnCare360 integrates Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and care gap closure into a single workflow. This unified approach supports the ACCESS Model’s emphasis on ongoing, technology-enabled chronic care rather than episodic office visits. Care coordinators can manage patients enrolled in multiple ACCESS tracks simultaneously, enhancing efficiency and clinical outcomes.
Measuring ROI and Outcomes with OnCare360
The ACCESS Model’s Outcome-Aligned Payments (OAPs) tie reimbursement to measurable health improvements, such as a 10 mmHg reduction in blood pressure or symptom reductions on validated tools. OnCare360 provides real-time tracking of patient progress toward these goals through dashboards that display the percentage of enrolled patients meeting performance metrics. These insights are critical for ensuring organizations qualify for full payment under the model’s thresholds.
Automated tools further simplify financial management by tracking patient interaction time, generating audit-ready documentation, and producing billing reports ready for submission. This reduces the administrative burden of managing multiple payment streams, including OAPs for the first 12 months of care, continuation payments at reduced rates, and co-management payments from referring clinicians. Rigorous enrollment safeguards and eligibility checks minimize the risk of recoupments.
OnCare360 also offers a specialized ROI calculator to help organizations estimate financial performance based on the clinical tracks they implement. This tool accounts for the payment structure, performance thresholds, and rural adjustment factors of the ACCESS Model. Additionally, the platform supports the collection and tracking of Patient-Reported Outcomes (PROs), such as pain and functional scores for musculoskeletal conditions and WHODAS 2.0 scores for behavioral health. By establishing baselines early and monitoring progress consistently, organizations can demonstrate the clinical improvements rewarded by CMS, laying the groundwork for long-term success in value-based care.
Preparing for the CMS ACCESS Model
The CMS ACCESS Model marks a major change in how Medicare reimburses chronic care, shifting from activity-based billing to payments tied to measurable clinical outcomes. Organizations that start preparing now - well ahead of the July 5, 2026 launch - will position themselves to secure enrollment and build the necessary foundation for success.
The first step in preparation is confirming Medicare Part B enrollment. This can be done through PECOS, as ACCESS applications require verified enrollment. Additionally, every participating organization must appoint a Medicare-enrolled physician as the Clinical Director to oversee care quality, compliance, and clinical governance.
Next, determine which clinical track aligns with your organization's expertise. The four available tracks - Early Cardio-Kidney-Metabolic Risk, Established Cardio-Kidney-Metabolic Disease, Chronic Musculoskeletal Pain, and Behavioral Health Conditions - address chronic conditions that impact over 66% of Medicare beneficiaries. By December 2025, more than 500 technology-enabled care organizations had already submitted intent-to-apply forms. Ensure your digital tools comply with HIPAA and FDA standards and establish secure data exchange pathways.
Submitting the ACCESS Model Interest Form on the CMS website is a critical step to receive updates and application notifications. Applications for the initial performance period are due by April 1, 2026, with rolling applications accepted through 2033 for later start dates. Additionally, develop co-management workflows with referring clinicians to bill $30 per review and a $10 onboarding fee every four months.
Lastly, CMS will maintain a public participant directory featuring risk-adjusted clinical outcomes to help patients make informed decisions. This transparency highlights the importance of strong clinical protocols and consistent outcome tracking from the outset. Organizations that prioritize compliant technology, efficient care coordination, and measurable results will be well-positioned to benefit from both the financial incentives and improved patient care this model offers.
FAQs
What are the key advantages of the CMS ACCESS Model for healthcare providers?
The CMS ACCESS (Advancing Chronic Care with Effective, Scalable Solutions) Model introduces a value-based payment approach designed to reward measurable health improvements rather than the volume of services delivered. For providers managing chronic conditions, this means predictable, recurring payments tied to tangible outcomes, such as improved blood pressure levels or a reduction in diabetes-related complications. This structure gives clinicians the freedom to choose the tools and care strategies that best align with each patient’s needs.
As a voluntary, 10-year program, the model provides a pathway to value-based care that can adapt to different practice sizes and capabilities. It offers new reimbursement opportunities, including payments that support coordinated, team-based care, while aiming to enhance patient outcomes and lower overall Medicare spending. By incorporating technology-driven solutions - such as remote patient monitoring and virtual visits - the model equips practices to address the rising demand for digital health services, all while improving operational efficiency and financial performance.
How does the CMS ACCESS Model ensure patient privacy and safety compliance?
The CMS ACCESS (Advancing Chronic Care with Effective, Scalable Solutions) Model prioritizes compliance with federal privacy and safety standards by mandating that all participants adhere to stringent regulatory requirements. To participate, organizations must be enrolled in Medicare Part B and designate a physician Clinical Director. This individual is responsible for overseeing care quality while ensuring compliance with both federal and state regulations.
Key safeguards include adherence to HIPAA privacy and security standards to protect patient health information, along with meeting any relevant FDA requirements for digital health tools. CMS maintains these standards through secure data submissions, continuous oversight, and routine audits, ensuring that care delivery and technology consistently align with federal safety and privacy protocols.
What outcome measures are required for each clinical track in the CMS ACCESS Model?
The CMS ACCESS Model is organized into four distinct clinical tracks: early cardio-kidney-metabolic, cardio-kidney-metabolic, musculoskeletal, and behavioral health. Each track links payment incentives to achieving specific outcome measures and targets, which participants must meet to succeed within the model.
Although CMS has not disclosed a comprehensive list of outcome measures for each track, an example from the cardio-kidney-metabolic track is the management or improvement of blood pressure in patients with hypertension. Other possible measures might include HbA1c levels, estimated glomerular filtration rate (eGFR), pain scores, or PHQ-9 scores, depending on the clinical focus of the track. However, these additional metrics have not been officially confirmed.
Participants must adhere to the track-specific outcome targets, though the complete set of measures remains under wraps for now.
CMS ACCESS Model: 4 Clinical Tracks Comparison Chart
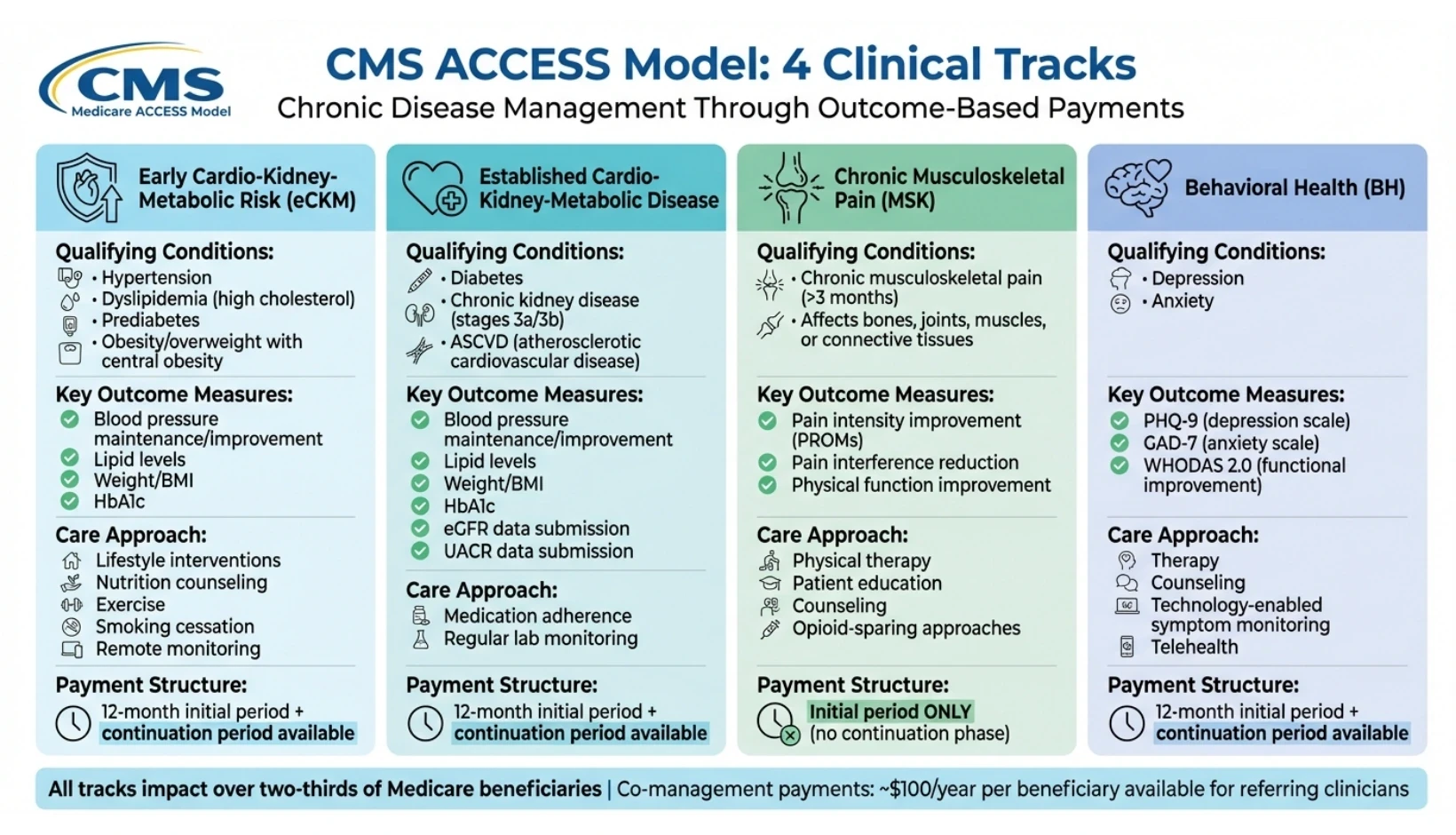
The CMS ACCESS Model organizes care into four distinct clinical tracks, each designed to address chronic conditions that impact over two-thirds of individuals enrolled in Original Medicare. These tracks require providers to manage all qualifying conditions within a given category, ensuring a coordinated, patient-centered approach. Payments are linked to measurable health improvements from each patient's baseline, making accurate and consistent outcome tracking a fundamental requirement. Below is an overview of the clinical tracks, their target conditions, and the associated goals.
Early Cardio-Kidney-Metabolic Risk Track
This track emphasizes early detection and risk management, aiming to intervene before chronic diseases fully develop. It focuses on conditions such as hypertension, dyslipidemia (high cholesterol), prediabetes, and obesity or overweight with signs of central obesity. The approach includes lifestyle interventions such as nutrition counseling, exercise guidance, smoking cessation, and remote monitoring through devices that track blood pressure and weight.
Key outcome measures include maintaining or improving clinical biomarkers like blood pressure, lipid levels, weight (or BMI), and hemoglobin A1c (HbA1c). Providers must establish baseline metrics and demonstrate measurable improvements or stability over time. This track is particularly well-suited for organizations with established wellness and preventive care programs. For more insights on optimizing these initiatives, visit our learning center.
Established Cardio-Kidney-Metabolic Disease Track
Building on the early risk management track, this category addresses patients with more advanced chronic conditions, including diabetes, chronic kidney disease (stages 3a and 3b), and atherosclerotic cardiovascular disease (ASCVD). The focus is on managing these conditions through medication adherence and regular monitoring of lab values.
Outcome measures are similar to the Early CKM Track - improvements in blood pressure, lipid levels, weight, and HbA1c - but with additional requirements. Providers must also submit detailed data on estimated glomerular filtration rate (eGFR) and urine albumin-creatinine ratio (UACR) for patients with chronic kidney disease or diabetes. This added layer of data collection underscores the need for detailed clinical oversight and a structured care approach.
Chronic Musculoskeletal Pain Track
This track targets chronic musculoskeletal pain lasting longer than three months, which can affect bones, joints, muscles, or connective tissues. Treatment strategies include physical therapy, patient education, counseling, and opioid-sparing approaches. Unlike the metabolic tracks, this track relies entirely on Patient Reported Outcome Measures (PROMs) to evaluate success.
Outcome measures focus on improvements in pain intensity, the impact of pain on daily activities, and overall physical function. Providers are expected to achieve meaningful improvements within the initial treatment period, as this track does not include a follow-up continuation phase. It is particularly suited for organizations with strong rehabilitation and pain management programs.
Behavioral Health Conditions Track
This track is designed to manage depression and anxiety through technology-enabled symptom monitoring and treatment adherence. Care delivery includes therapy, counseling, and the use of standardized tools to track symptoms over time.
Outcome measures are based on validated scales, including the Patient Health Questionnaire (PHQ-9) for depression and the Generalized Anxiety Disorder scale (GAD-7) for anxiety. Additionally, providers must submit data from the WHODAS 2.0 12-item scale to assess overall functional improvement. Given the episodic nature of behavioral health issues, this track requires robust systems for telehealth, secure communication, and asynchronous monitoring to ensure consistent patient engagement and progress tracking.
Clinical Track | Qualifying Conditions | Key Outcome Measures |
|---|---|---|
Early CKM (eCKM) | Hypertension, dyslipidemia, prediabetes, obesity/overweight | Maintenance or improvement in BP, lipids, weight/BMI, and HbA1c |
Established CKM | Diabetes, CKD (3a/3b), ASCVD (heart disease) | Maintenance/improvement in BP, lipids, weight, HbA1c; submission of eGFR and UACR data |
Musculoskeletal (MSK) | Chronic musculoskeletal pain (>3 months) | Improvements in pain intensity, interference, and physical function via PROMs |
Behavioral Health (BH) | Depression, anxiety | Symptom improvement (PHQ-9, GAD-7) and functional gains (WHODAS 2.0) |
How Outcome-Aligned Payments Work
The ACCESS Model introduces a new approach called Outcome-Aligned Payments (OAPs), which ties recurring payments to measurable clinical outcomes. To receive full payment, providers must meet specific clinical targets for a significant portion of their enrolled patients. Unlike the traditional fee-for-service system that rewards individual patient successes, the Centers for Medicare & Medicaid Services (CMS) bases these payments on the percentage of patients achieving their outcome goals, with minimum thresholds that increase each year of participation. This payment structure is designed to support ongoing care by enabling continuous monitoring and interventions between office visits.
"By rewarding outcomes rather than defined activities (or volume of services delivered), ACCESS gives clinicians greater flexibility to deliver modern technology-supported care in ways that best improve patient health." - CMS
Most tracks under the model include an initial 12-month care period with higher payment rates. After that, providers can opt for a continuation period at a reduced rate, reflecting the lower resource needs once care is established. For patients enrolled in multiple tracks with the same provider, CMS applies a discount to the total payment to account for administrative efficiencies. The Musculoskeletal (MSK) track, which focuses on addressing chronic pain, is an exception - it offers only the initial care period and no continuation phase. This framework highlights how payment tiers and performance thresholds create financial incentives while maintaining a focus on patient outcomes.
Payment Tiers and Performance Thresholds
The model structures payment tiers around performance thresholds, which represent the minimum percentage of enrolled patients who must meet their clinical targets for providers to receive full payment. These thresholds increase annually to encourage ongoing improvement and engagement. The focus is on measurable progress from each patient's baseline. For instance, a patient with severe hypertension who lowers their systolic blood pressure by 10 mmHg contributes to the threshold, even if their blood pressure hasn’t yet reached the ideal range.
Co-Management Payments
Beyond outcome-aligned payments, the ACCESS Model includes co-management payments for primary care or referring clinicians who collaborate with ACCESS organizations. These payments are approximately $30 for each documented review, with an additional $10 onboarding payment available the first time a clinician helps set up a beneficiary. Clinicians can bill for co-management once every four months per beneficiary, with payments totaling around $100 per beneficiary annually. To qualify, clinicians must review the ACCESS Care Update and document at least one care coordination action in the electronic health record - such as updating a problem list, making a medication change, initiating new monitoring instructions, or providing a referral. There is no cost-sharing for beneficiaries, and advance consent is not required. Starting in 2028, ACCESS payments will be included in ACO REACH and Medicare Shared Savings Program benchmark calculations, but for 2026 and 2027, these payments will not impact ACO benchmarks.
Payment Comparison by Track
Although CMS has not yet provided specific base OAP dollar amounts by track as of December 2025, the payment structure varies depending on the complexity and duration of care. Below is an overview of the general framework:
Track | Initial Care Period | Continuation Period | Co-Management | Key Payment Considerations |
|---|---|---|---|---|
Early CKM (eCKM) | 12 months at full rate | Available at reduced rate | $100/year | Focus on prevention; lower clinical complexity |
Established CKM | 12 months at full rate | Available at reduced rate | $100/year | Higher clinical complexity; requires eGFR/UACR data submission |
Musculoskeletal (MSK) | Initial period only | Not available | $100/year | Designed for pain resolution; no long-term continuation |
Behavioral Health (BH) | 12 months at full rate | Available at reduced rate | $100/year | Episodic care; requires telehealth and remote monitoring |
For rural patients enrolled in qualifying tracks, a fixed adjustment is applied to encourage access in underserved areas. Additionally, participants can choose to waive beneficiary cost-sharing for OAPs to promote engagement.
Implementing the CMS ACCESS Model with OnCare360
OnCare360 aligns seamlessly with the CMS ACCESS performance framework, offering a comprehensive solution to integrate care delivery, compliance, and ROI measurement for value-based care initiatives. The platform provides the necessary infrastructure to meet CMS ACCESS operational and compliance standards while scaling between-visit care. By consolidating outcome tracking, API-based reporting, care coordination workflows, and audit-ready documentation, OnCare360 supports all four ACCESS clinical tracks - Early CKM, Established CKM, Musculoskeletal Pain, and Behavioral Health - without requiring separate workflows for each program.
How OnCare360 Supports CMS ACCESS Requirements
OnCare360 simplifies compliance with CMS standards through features like integrated data exchange and preloaded compliance checks, ensuring adherence to API and HIPAA requirements while reducing manual documentation efforts. Real-time dashboards provide Clinical Directors with oversight of patient outcomes, intervention timelines, and progress against annual performance thresholds outlined by the ACCESS Model. The platform also systematically gathers baseline clinical measures - such as HbA1c, blood pressure, and weight - and validated Patient-Reported Outcome Measures (PROMs) like PHQ-9 for depression and GAD-7 for anxiety, which are essential for tracking improvements from each patient’s starting point.
For co-management billing, OnCare360 automates the distribution of ACCESS Care Updates to referring clinicians at key stages: treatment initiation, completion, and clinical milestones. These updates enable primary care providers to document care coordination actions, such as updating problem lists, adjusting treatment plans, or initiating new monitoring protocols. This documentation supports billing of the $30 co-management payment (plus a $10 onboarding modifier for first-time setups) every four months per beneficiary. Secure, automated workflows ensure compliance with CMS interoperability requirements while minimizing administrative workload.
Beyond compliance, OnCare360 enhances care delivery, making it easier to manage high-risk patient populations effectively.
Scaling Between-Visit Care with OnCare360
Once CMS requirements are met, OnCare360’s scalable tools enable care teams to efficiently manage chronic conditions, which impact nearly two-thirds of Medicare beneficiaries. By leveraging AI-driven care coordination, the platform identifies prioritization cues, risk alerts, and documentation suggestions, while licensed clinicians make final care decisions and interventions. This collaborative approach allows smaller care teams to oversee large patient panels without compromising quality.
The platform’s medical-grade cellular devices eliminate setup hurdles by automatically transmitting critical health data - such as blood pressure, glucose, weight, and pulse oximetry - directly to the care platform. These devices don’t require patient Wi-Fi or app downloads, ensuring continuous data flow. This real-time visibility aligns with the ACCESS Model’s focus on between-visit care, enabling timely interventions when clinical metrics deviate from target ranges.
OnCare360 integrates Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and care gap closure into a single workflow. This unified approach supports the ACCESS Model’s emphasis on ongoing, technology-enabled chronic care rather than episodic office visits. Care coordinators can manage patients enrolled in multiple ACCESS tracks simultaneously, enhancing efficiency and clinical outcomes.
Measuring ROI and Outcomes with OnCare360
The ACCESS Model’s Outcome-Aligned Payments (OAPs) tie reimbursement to measurable health improvements, such as a 10 mmHg reduction in blood pressure or symptom reductions on validated tools. OnCare360 provides real-time tracking of patient progress toward these goals through dashboards that display the percentage of enrolled patients meeting performance metrics. These insights are critical for ensuring organizations qualify for full payment under the model’s thresholds.
Automated tools further simplify financial management by tracking patient interaction time, generating audit-ready documentation, and producing billing reports ready for submission. This reduces the administrative burden of managing multiple payment streams, including OAPs for the first 12 months of care, continuation payments at reduced rates, and co-management payments from referring clinicians. Rigorous enrollment safeguards and eligibility checks minimize the risk of recoupments.
OnCare360 also offers a specialized ROI calculator to help organizations estimate financial performance based on the clinical tracks they implement. This tool accounts for the payment structure, performance thresholds, and rural adjustment factors of the ACCESS Model. Additionally, the platform supports the collection and tracking of Patient-Reported Outcomes (PROs), such as pain and functional scores for musculoskeletal conditions and WHODAS 2.0 scores for behavioral health. By establishing baselines early and monitoring progress consistently, organizations can demonstrate the clinical improvements rewarded by CMS, laying the groundwork for long-term success in value-based care.
Preparing for the CMS ACCESS Model
The CMS ACCESS Model marks a major change in how Medicare reimburses chronic care, shifting from activity-based billing to payments tied to measurable clinical outcomes. Organizations that start preparing now - well ahead of the July 5, 2026 launch - will position themselves to secure enrollment and build the necessary foundation for success.
The first step in preparation is confirming Medicare Part B enrollment. This can be done through PECOS, as ACCESS applications require verified enrollment. Additionally, every participating organization must appoint a Medicare-enrolled physician as the Clinical Director to oversee care quality, compliance, and clinical governance.
Next, determine which clinical track aligns with your organization's expertise. The four available tracks - Early Cardio-Kidney-Metabolic Risk, Established Cardio-Kidney-Metabolic Disease, Chronic Musculoskeletal Pain, and Behavioral Health Conditions - address chronic conditions that impact over 66% of Medicare beneficiaries. By December 2025, more than 500 technology-enabled care organizations had already submitted intent-to-apply forms. Ensure your digital tools comply with HIPAA and FDA standards and establish secure data exchange pathways.
Submitting the ACCESS Model Interest Form on the CMS website is a critical step to receive updates and application notifications. Applications for the initial performance period are due by April 1, 2026, with rolling applications accepted through 2033 for later start dates. Additionally, develop co-management workflows with referring clinicians to bill $30 per review and a $10 onboarding fee every four months.
Lastly, CMS will maintain a public participant directory featuring risk-adjusted clinical outcomes to help patients make informed decisions. This transparency highlights the importance of strong clinical protocols and consistent outcome tracking from the outset. Organizations that prioritize compliant technology, efficient care coordination, and measurable results will be well-positioned to benefit from both the financial incentives and improved patient care this model offers.
FAQs
What are the key advantages of the CMS ACCESS Model for healthcare providers?
The CMS ACCESS (Advancing Chronic Care with Effective, Scalable Solutions) Model introduces a value-based payment approach designed to reward measurable health improvements rather than the volume of services delivered. For providers managing chronic conditions, this means predictable, recurring payments tied to tangible outcomes, such as improved blood pressure levels or a reduction in diabetes-related complications. This structure gives clinicians the freedom to choose the tools and care strategies that best align with each patient’s needs.
As a voluntary, 10-year program, the model provides a pathway to value-based care that can adapt to different practice sizes and capabilities. It offers new reimbursement opportunities, including payments that support coordinated, team-based care, while aiming to enhance patient outcomes and lower overall Medicare spending. By incorporating technology-driven solutions - such as remote patient monitoring and virtual visits - the model equips practices to address the rising demand for digital health services, all while improving operational efficiency and financial performance.
How does the CMS ACCESS Model ensure patient privacy and safety compliance?
The CMS ACCESS (Advancing Chronic Care with Effective, Scalable Solutions) Model prioritizes compliance with federal privacy and safety standards by mandating that all participants adhere to stringent regulatory requirements. To participate, organizations must be enrolled in Medicare Part B and designate a physician Clinical Director. This individual is responsible for overseeing care quality while ensuring compliance with both federal and state regulations.
Key safeguards include adherence to HIPAA privacy and security standards to protect patient health information, along with meeting any relevant FDA requirements for digital health tools. CMS maintains these standards through secure data submissions, continuous oversight, and routine audits, ensuring that care delivery and technology consistently align with federal safety and privacy protocols.
What outcome measures are required for each clinical track in the CMS ACCESS Model?
The CMS ACCESS Model is organized into four distinct clinical tracks: early cardio-kidney-metabolic, cardio-kidney-metabolic, musculoskeletal, and behavioral health. Each track links payment incentives to achieving specific outcome measures and targets, which participants must meet to succeed within the model.
Although CMS has not disclosed a comprehensive list of outcome measures for each track, an example from the cardio-kidney-metabolic track is the management or improvement of blood pressure in patients with hypertension. Other possible measures might include HbA1c levels, estimated glomerular filtration rate (eGFR), pain scores, or PHQ-9 scores, depending on the clinical focus of the track. However, these additional metrics have not been officially confirmed.
Participants must adhere to the track-specific outcome targets, though the complete set of measures remains under wraps for now.

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?


