How Between-Visit Care Reduces Avoidable Hospitalizations
OnCare360
Nov 9, 2025
Preventable hospitalizations cost the U.S. healthcare system over $25 billion annually, often resulting from gaps in outpatient care for conditions like diabetes, COPD, and heart failure. Between-visit care, which includes Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Transitional Care Management (TCM), helps address these gaps by enabling continuous monitoring, early intervention, and improved care coordination. This article explores how structured between-visit care reduces acute episodes, improves patient outcomes, and supports value-based care models by lowering hospital admissions and readmissions.
How Between-Visit Care Reduces Hospital Admissions
Between-visit care programs play a crucial role in identifying potential health issues early, reducing the likelihood of emergencies. By maintaining consistent communication with patients and monitoring their health in real time, these initiatives effectively close the gaps between office visits. This proactive approach minimizes complications, curtails emergency room visits, and helps patients avoid hospital stays. Let’s explore how continuous coordination, remote monitoring, and focused transitional care contribute to these outcomes.
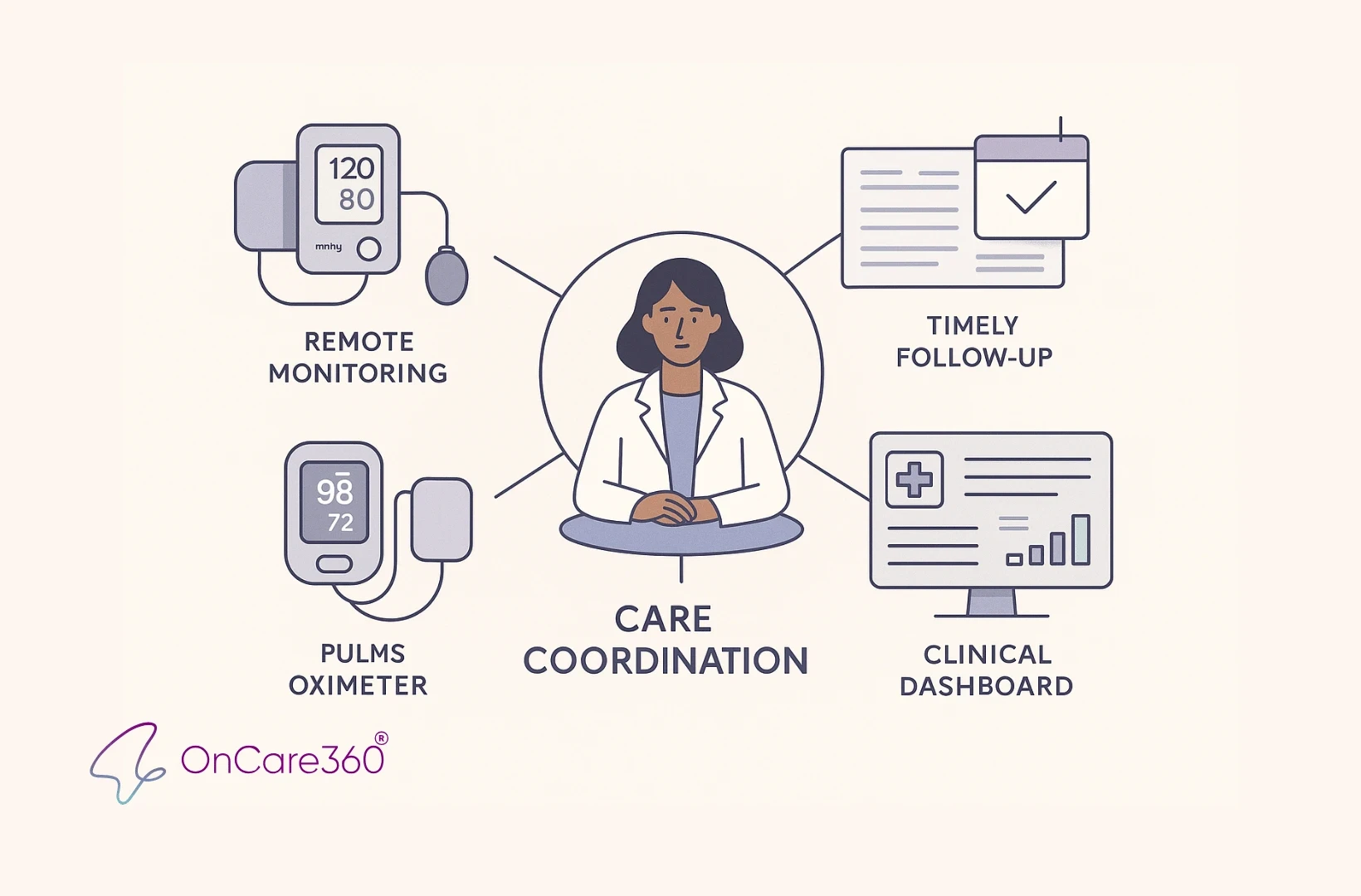
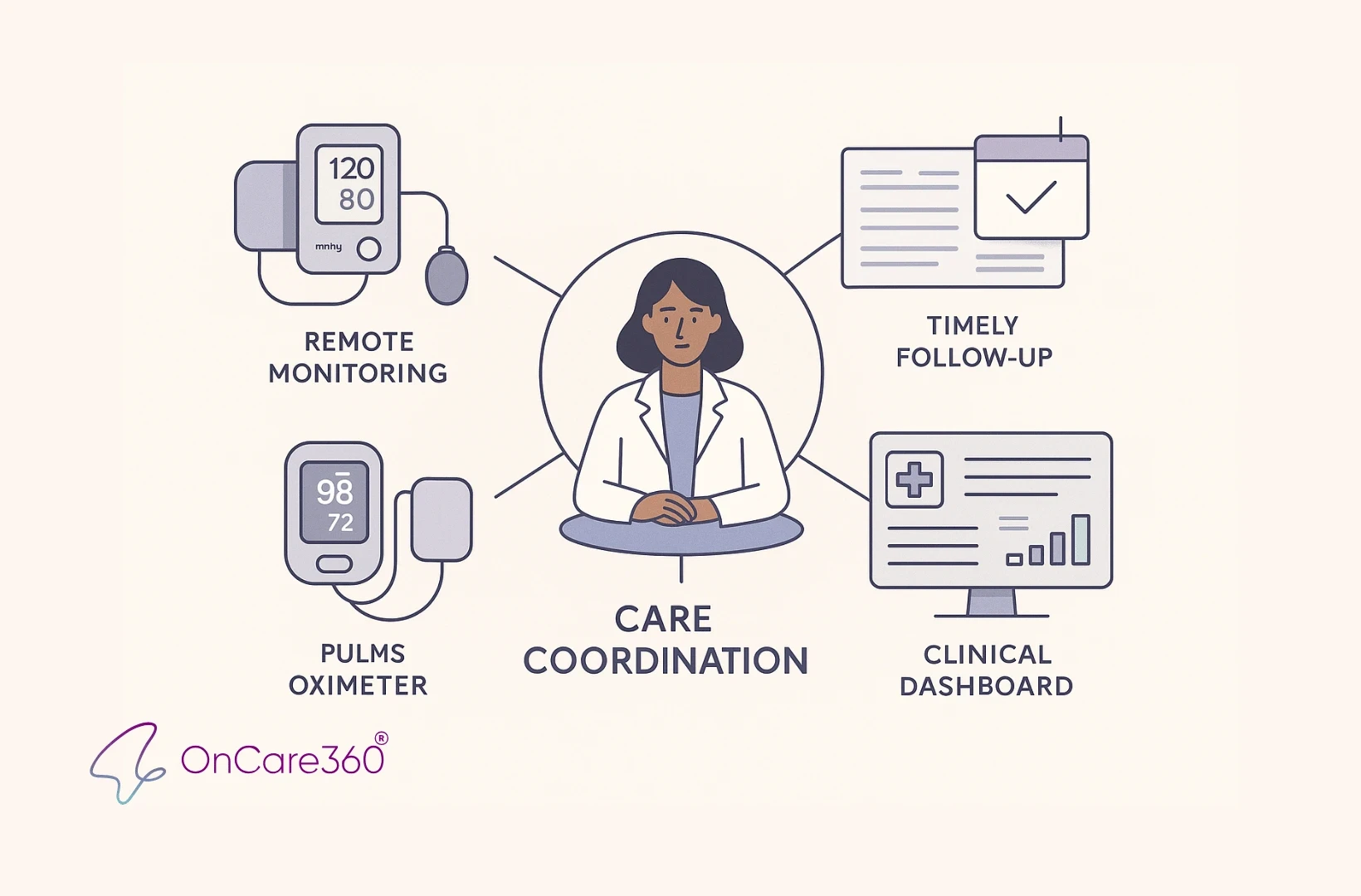
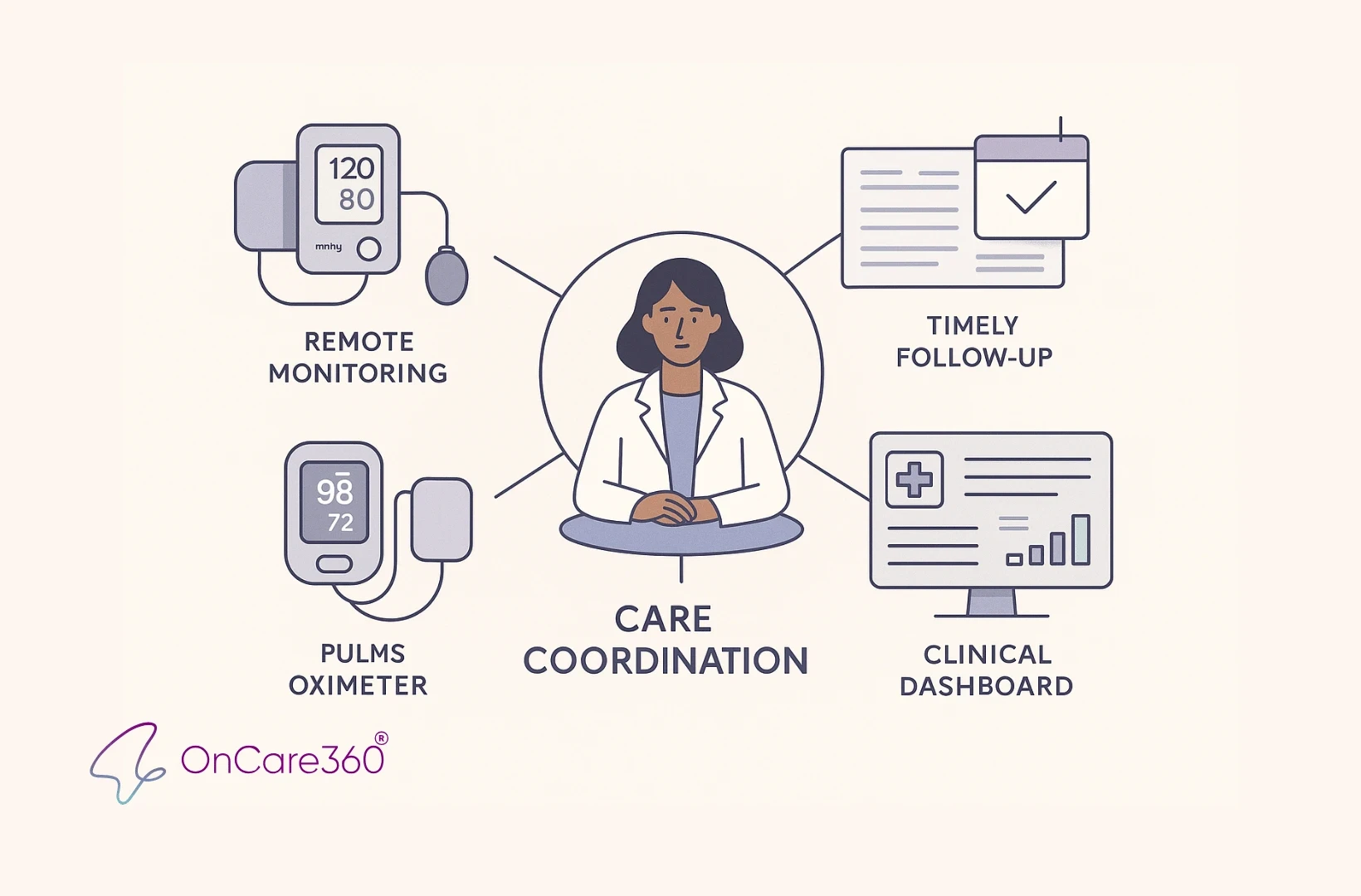
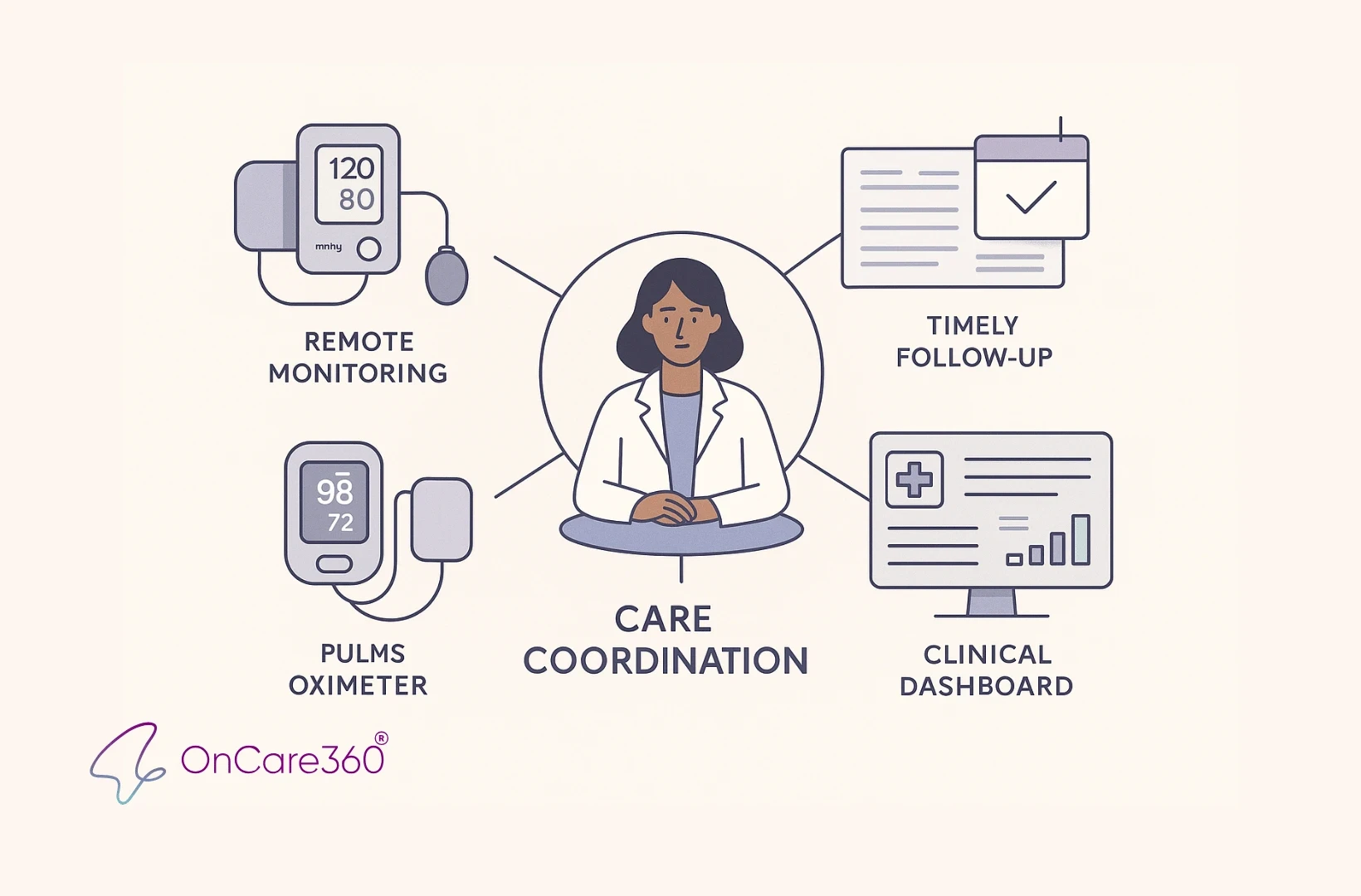
Continuous Care Coordination
At the heart of between-visit care lies structured care plans and regular communication between patients and providers. Rather than waiting for the next scheduled appointment, care teams actively engage with patients to monitor symptoms, reconcile medications, coordinate follow-ups, and address barriers like transportation or food insecurity. This constant engagement allows for early detection of health changes, enabling timely adjustments to care plans and preemptive interventions.
The impact of coordinated care is significant. Studies show that hospitalization rates can drop by 25–60% through effective care coordination. For instance, a Federally Qualified Health Center implementing a Chronic Care Management (CCM) program reported a 60% reduction in emergency room visits. Similarly, patients with congestive heart failure (CHF) or chronic obstructive pulmonary disease (COPD) who had nine or more primary care visits were much less likely to require hospitalization, with odds ratios of 0.82 for CHF and 0.81 for COPD. Among the sickest Medicare beneficiaries, frequent primary care visits led to a 9% reduction in hospital days.
Consistent communication also fosters trust, encouraging patients to stick to their medications, report symptoms early, and adhere to treatment plans. In one CCM program, 71% of diabetic patients achieved better A1C levels through medication adherence support and lifestyle coaching.
Early Detection Through Remote Monitoring
Remote Patient Monitoring (RPM) provides real-time tracking of vital signs like blood pressure, heart rate, oxygen levels, and glucose levels. Automated systems flag significant deviations, alerting care teams to intervene before conditions escalate. This approach shifts care from being reactive to proactive, reducing the risk of emergencies.
Post-Discharge Support with Transitional Care Management (TCM)
The days and weeks following a hospital discharge are often filled with challenges, such as confusion over medications, missed follow-up appointments, or unaddressed symptoms - all of which can lead to readmissions. Transitional Care Management (TCM) addresses these issues by assigning a dedicated provider, such as a nurse or case manager, to oversee post-discharge care.
The benefits of structured post-discharge care are evident. For example, White Plains Hospital’s WPH Cares program demonstrated how timely follow-up can reduce readmission rates. From May 2021 to December 2022, registered nurses contacted patients within 24–48 hours of discharge to address medication questions, schedule follow-ups, and identify potential issues. As a result, median readmission rates dropped from 11.0% to 9.8% for all-cause readmissions. Disease-specific improvements were also striking, with CHF readmissions falling from 14.3% to 9.1%, COPD readmissions from 20.0% to 13.4%, and pneumonia readmissions from 14.9% to 14.0%.
Patients contacted within 24–48 hours were 1.2 times less likely to be readmitted - 6.8% compared to 8.2%. Among those reached, 76.6% needed reinforcement of discharge instructions, 51.5% sought advice on medical concerns, 21.7% required assistance with scheduling appointments, and 12.4% benefited from medication education. These findings highlight how focused support during the transitional period can significantly improve patient outcomes and reduce readmissions.
Gaps in Visit-Based Care Models
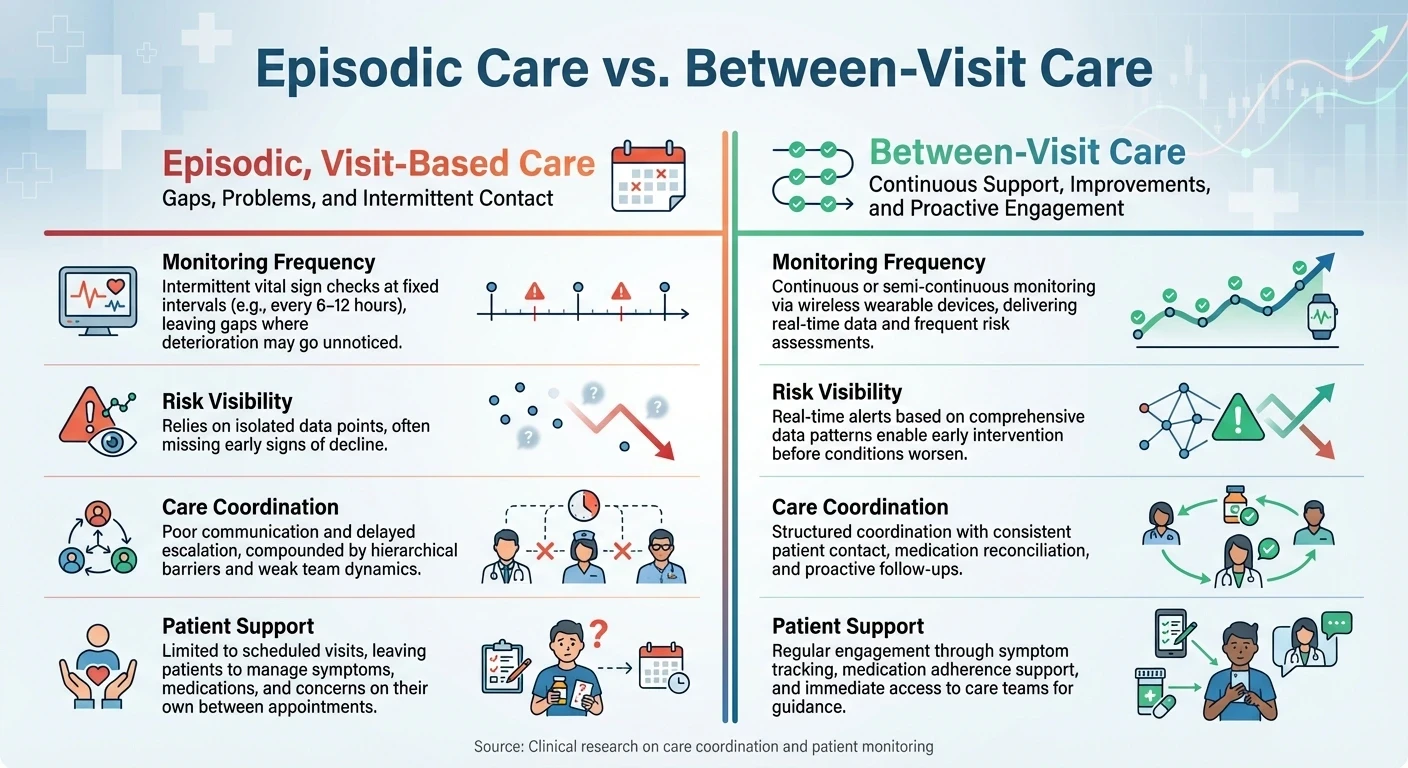
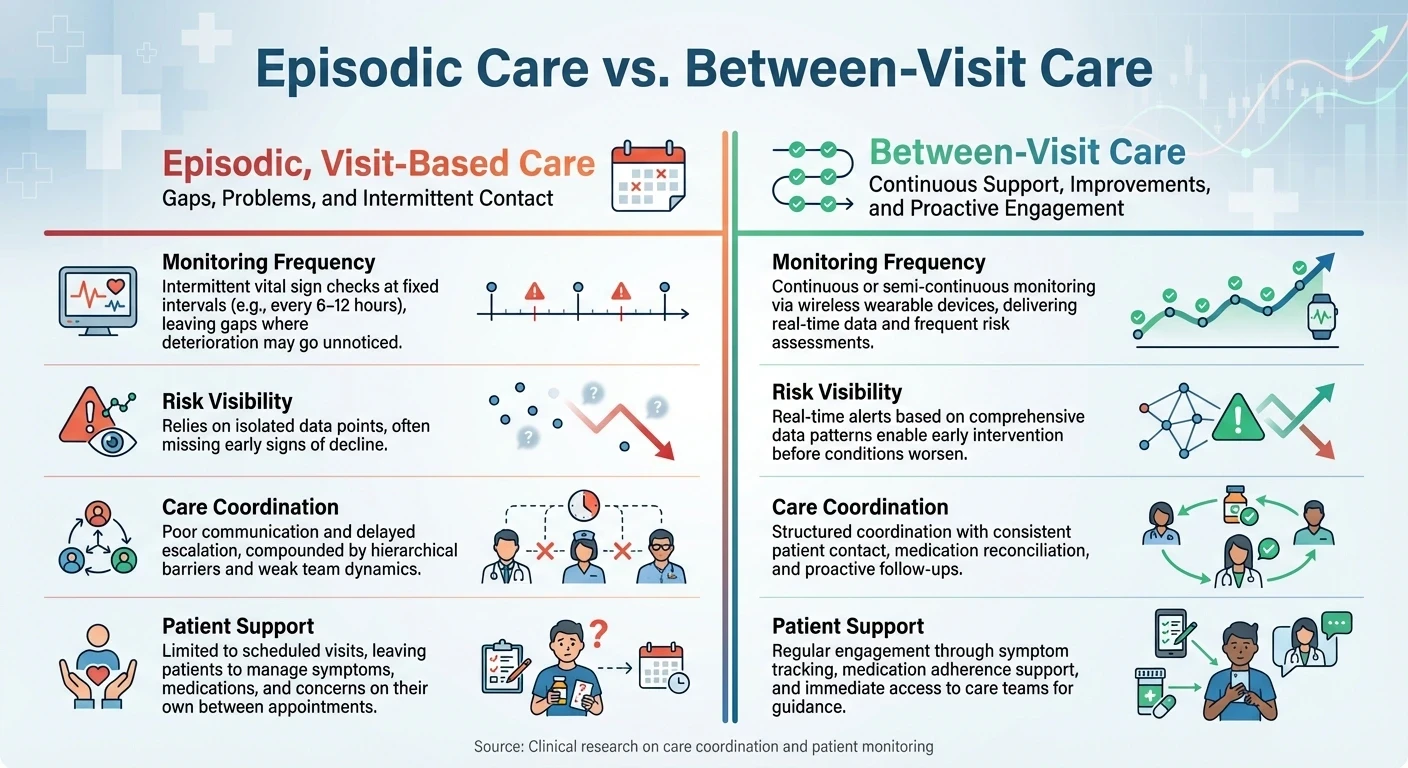
Episodic Care vs Between-Visit Care: Key Differences in Patient Monitoring
The traditional visit-based care model has inherent blind spots when it comes to monitoring patients, particularly those with chronic conditions. These gaps leave extended periods where a patient’s health can decline unnoticed, often resulting in emergency room visits or hospitalizations. Office visits alone cannot meet the ongoing needs of patients who require consistent attention and coordination. This highlights the importance of proactive, continuous monitoring strategies.
Problems with Episodic, Visit-Based Care
A significant drawback of visit-based care is its fragmented oversight. Patients with chronic conditions frequently see multiple specialists, but poor coordination among providers means no one has a complete view of the patient’s overall health. This lack of integration often results in medication conflicts, redundant procedures, and missed opportunities to address worsening conditions before they become critical.
Intermittent monitoring is another shortfall, as it creates periods where health deterioration can go unnoticed. Research indicates that protocols for recording vital signs are often not followed consistently. For example, the National Early Warning Score 2 (NEWS2) is frequently underestimated, with accurate assessments revealing a higher risk level in 27% of cases.
Additionally, delayed escalation is a recurring issue. Timely interventions are undermined, with full adherence to escalation protocols observed in only 8% of serious adverse events. Monitoring delays occurred in 81% of cases, and appropriate escalation for elevated early warning scores was implemented in just 60% of moderate-risk cases and 41% of high-risk cases. Even among patients with the highest risk scores, only half were reviewed by senior staff or a Medical Emergency Team. High patient volumes and the perception that moderately elevated scores wouldn’t change management often deter nurses from notifying physicians.
Additionally, delayed escalation is a recurring issue. Timely interventions are undermined, with full adherence to escalation protocols observed in only 8% of serious adverse events. Monitoring delays occurred in 81% of cases, and appropriate escalation for elevated early warning scores was implemented in just 60% of moderate-risk cases and 41% of high-risk cases. Even among patients with the highest risk scores, only half were reviewed by senior staff or a Medical Emergency Team. High patient volumes and the perception that moderately elevated scores wouldn’t change management often deter nurses from notifying physicians.
Episodic Care vs. Between-Visit Care
Continuous care offers clear advantages over episodic, visit-based models. The following table highlights key differences and demonstrates how between-visit care addresses the shortcomings of traditional approaches:
Aspect | Episodic, Visit-Based Care | Between-Visit Care |
|---|---|---|
Monitoring Frequency | Intermittent vital sign checks at fixed intervals (e.g., every 6–12 hours), leaving gaps where deterioration may go unnoticed | Continuous or semi-continuous monitoring via wireless wearable devices, delivering real-time data and frequent risk assessments |
Risk Visibility | Relies on isolated data points, often missing early signs of decline | Real-time alerts based on comprehensive data patterns enable early intervention before conditions worsen |
Care Coordination | Poor communication and delayed escalation, compounded by hierarchical barriers and weak team dynamics | Structured coordination with consistent patient contact, medication reconciliation, and proactive follow-ups |
Patient Support | Limited to scheduled visits, leaving patients to manage symptoms, medications, and concerns on their own between appointments | Regular engagement through symptom tracking, medication adherence support, and immediate access to care teams for guidance |
Recognizing these gaps is a critical step toward adopting more effective care models that prioritize continuous monitoring and patient-centered solutions.
Using CCM, RPM, and TCM to Reduce Hospitalizations
Integrating Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Transitional Care Management (TCM) into between-visit care programs can help identify early warning signs before emergencies occur. CCM lays the groundwork with ongoing care coordination, RPM provides real-time tracking of patient vitals, and TCM ensures smooth transitions after hospital discharge. Together, these programs work as a cohesive system to address gaps that often lead to preventable hospitalizations.
Chronic Care Management (CCM): Establishing the Framework
CCM provides a structured approach to managing patients with two or more chronic conditions expected to persist for at least 12 months. This program extends care beyond the clinic, focusing on medication reviews, personalized care plans, and proactive patient outreach. Care teams use comprehensive risk assessments, evaluating factors like social support and medication adherence, to identify patients most at risk for hospitalization.
Core elements of CCM include clear medication schedules, shared treatment plans, and self-management education. This is especially critical given that approximately two-thirds of Medicare beneficiaries manage multiple chronic conditions. Multidisciplinary teams customize care by integrating behavioral health into primary care settings and employing social work teams to address social determinants of health. These strategies significantly lower the likelihood of hospitalizations.
This foundational framework is further strengthened by RPM, which enables continuous tracking of patient health metrics.
Remote Patient Monitoring (RPM): Detecting Issues Early
RPM revolutionizes care by enabling real-time monitoring of patient vitals through connected devices such as blood pressure monitors and glucose meters. These devices transmit data directly to care teams, allowing them to identify trends and intervene early, often before complications arise. This approach is particularly beneficial for high-risk patients, including those recently discharged or those struggling with poorly managed chronic conditions.
For instance, a program monitoring patients with chronic heart disease through daily RPM saw a 37% reduction in hospital readmissions. Similarly, diabetes patients who received regular RPM reminders for submitting blood sugar levels and insulin usage achieved better glycemic control and fewer emergency room visits due to diabetic complications. Across various conditions, RPM has been shown to reduce hospital admissions, shorten hospital stays, and decrease emergency department visits in nearly 50% of studies, with significant results for chronic obstructive pulmonary disease (COPD).
While RPM provides continuous oversight, TCM ensures that patients transition safely back to their communities after hospital stays.
Transitional Care Management (TCM): Ensuring Smooth Transitions
TCM addresses the critical first 30 days after hospital discharge, a period when patients are highly vulnerable to readmission. Through structured workflows, including initial outreach, medication reconciliation, and timely follow-ups, TCM ensures continuity of care. This comprehensive support helps bridge communication gaps between hospital and primary care teams, reducing risks like medication errors, missed appointments, and rapid health declines.
Accountable Care Organizations (ACOs) that implement strong TCM programs often achieve 20-30% reductions in 30-day readmissions, along with fewer emergency department visits. The program also strengthens communication between providers and ensures patients receive clear discharge instructions. Together, CCM, RPM, and TCM form an integrated care continuum that reduces hospital readmissions and enhances patient outcomes.
Building Scalable Between-Visit Care with OnCare360
OnCare360 builds on the principles of continuous care coordination and real-time monitoring, offering a platform designed to scale efficiently. Managing Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Transitional Care Management (TCM) requires a robust operational framework to handle ongoing monitoring, documentation, compliance, and care coordination. OnCare360 delivers this through a unified system tailored for physician groups and value-based organizations that care for high-risk chronic patients between clinic visits. By combining AI-driven workflow automation with certified care teams and medical-grade monitoring devices, the platform reduces operational strain while maintaining clinical quality and audit readiness. Below, we explore how OnCare360's integrated features support scalable and compliant care delivery.
Unified Care Management Platform
OnCare360 consolidates key care management functions - including CCM, RPM, TCM, and behavioral health - into a single, streamlined workflow. This eliminates the inefficiencies of fragmented systems by enabling care teams to work within one platform that handles patient enrollment, care plan execution, medication reconciliation, vital sign monitoring, and billing documentation in real time. By centralizing these functions, the platform minimizes missed interventions and redundant efforts, reinforcing the continuous care model essential for reducing preventable hospitalizations.
The platform also incorporates cellular medical-grade devices that automatically transmit vital signs without requiring any setup by patients. These devices feed data directly into the care coordination system, allowing clinical teams to monitor high-risk patients consistently and intervene before complications arise. For practices managing large populations of patients with chronic conditions, this infrastructure removes technical barriers to RPM adoption and ensures a steady flow of data, regardless of patients' familiarity with technology.
AI-Driven Risk Prioritization and Monitoring
OnCare360 leverages AI-powered care coordination to identify risk signals, prioritize tasks, and provide documentation suggestions - all while keeping licensed clinicians in full control of care decisions and interventions. The system analyzes incoming vital signs, flags concerning trends, and routes alerts to care coordinators based on established clinical protocols and patient acuity levels. This approach enables small care teams to efficiently manage large patient populations without compromising clinical oversight or quality.
The AI system also automates routine tasks such as logging communications, updating care plans, and tracking billing time. This allows care coordinators to focus on patient engagement and timely interventions while maintaining the documentation standards necessary for audits and reducing the risk of clawbacks. By balancing automation with clinical oversight, OnCare360 ensures that care teams can manage growing patient panels effectively while maintaining high standards of care.
Scalability and Compliance for Value-Based Care
OnCare360 is designed to scale seamlessly across specialties such as primary care, cardiology, nephrology, and endocrinology, without requiring extensive customizations or IT overhauls. The cloud-based platform integrates with existing EHR systems, enabling quick deployment across multi-site organizations. Practices can start with a small pilot group and gradually expand as they demonstrate improvements in patient engagement, vital sign stability, and reductions in acute care episodes.
The platform also includes robust enrollment safeguards and eligibility checks, ensuring that billing aligns with clinical criteria rather than aggressive enrollment strategies. Monthly billing reports, denial management support, and clear documentation summaries simplify administrative tasks for practice managers and revenue cycle management (RCM) teams, improving clean-claim rates. For organizations involved in TEAM, ACCESS, or other value-based payment programs, OnCare360 provides the tools needed for continuous monitoring, care gap closure, and outcome tracking - key elements for success in shared savings and risk-adjusted payment models.
Measuring Outcomes and ROI from Between-Visit Care
To truly understand the value of continuous between-visit care, it's essential to evaluate both patient outcomes and financial returns. This requires analyzing lagging indicators, such as hospitalizations and emergency department visits, alongside leading indicators that help identify emerging risks early.
Key Metrics for Reducing Preventable Hospitalizations
Metrics like all-cause hospitalization and emergency department visit rates are critical in assessing whether between-visit care helps prevent avoidable admissions. However, relying solely on 30-day readmission rates can be misleading, as some acute care returns are reclassified during this period.
A more thorough evaluation includes financial and process metrics that reflect overall care costs and early warning signs of health deterioration. Establishing baseline metrics before implementing a program is vital for tracking improvements over time.
Real-world examples highlight the effectiveness of between-visit care. In 2023, Medicare Advantage patients in Humana's value-based care arrangements experienced 32.1% fewer inpatient hospital admissions and 11.6% fewer emergency department visits compared to those in non–value-based care models. Similarly, a 2024 study by the VillageMD Research Institute revealed that patients who maintained regular engagement with their primary care providers saw lower hospital admission rates. In contrast, patients with chronic conditions like COPD and congestive heart failure who had fewer visits experienced an increase in admissions.
"Our report paints a clear picture: value-based practices deliver better patient experiences and health outcomes. Patients spend more time with their primary care clinician, which means more preventive care and better management of chronic diseases, like diabetes and high blood pressure. Seniors in value-based care models receive the care they deserve with a clinician who holistically understands their care needs." - Kate Goodrich, MD, MHS, Chief Medical Officer, Humana
Beyond clinical improvements, it's equally important to measure the financial and operational impact of between-visit care.
Calculating Financial and Clinical ROI
Once outcomes are measured, calculating return on investment (ROI) helps validate the financial viability of between-visit care programs. This involves comparing revenue gains and cost reductions against the total program investment. A good starting point is establishing baseline data, such as average administrative time per patient, revenue generated from care management billing codes, and costs related to missed appointments.
Direct financial benefits include increased reimbursements from care management billing codes and revenue recovery from fewer no-shows. Patient engagement platforms can reduce no-show rates by 20–40%, a significant improvement considering that no-shows account for 15–30% of lost revenue in small practices. For instance, a practice generating $500,000 annually with a 20% no-show rate could recover approximately $30,000 each year by improving appointment adherence.
Indirect benefits also play a major role, particularly in reducing acute care utilization. Chronic conditions drive 85% of total healthcare costs, making their management a key financial consideration. Additionally, evaluating the broader value on investment (VOI) - including enhanced patient experience, improved clinical outcomes, and increased care team satisfaction - provides a more comprehensive view of long-term program sustainability, even when these benefits aren't immediately visible in financial statements.
Common ROI pitfalls include overlooking indirect costs, overestimating patient engagement levels, and failing to account for quality improvements. Accurate ROI assessments should consider the shift from volume-based to value-based care and the cumulative benefits of sustained patient engagement. Practices using robust patient engagement platforms report a 3-year ROI ranging from 6:1 to 15:1, along with reduced administrative costs and improved patient retention.
Conclusion: Reducing Hospitalizations with OnCare360
Preventable hospitalizations not only strain resources but also disrupt the continuity of patient care. Between-visit care programs have demonstrated their ability to lower such admissions, enhance chronic disease management, and increase patient satisfaction. However, many healthcare practices face challenges like fragmented tools, inconsistent processes, and the operational difficulties of scaling these programs effectively.
OnCare360 addresses these hurdles by offering a streamlined platform that integrates care coordination, AI-powered prioritization, and medical-grade home monitoring. This unified system eliminates the inefficiencies caused by disconnected tools, which often lead to gaps in care transitions. Certified care coordinators, supported by standardized pathways and real-time patient data, enable practices to proactively identify high-risk patients and intervene before conditions escalate.
The platform's AI-driven automation, combined with clinical oversight, allows small teams to manage larger patient populations while maintaining audit-ready documentation. Its cellular medical-grade devices simplify patient engagement, providing continuous monitoring of vital signs without requiring Wi-Fi or complex setups. This seamless flow of real-time data enhances communication across care settings, ensures timely medication reconciliation, and strengthens patient safety - all critical components of effective care continuity. These operational improvements align directly with the goals of value-based care.
For physician groups and organizations focused on value-based models, OnCare360 delivers measurable improvements across clinical, operational, and financial domains. By optimizing care workflows and reducing emergency visits, the platform supports the shift toward value-based care. Additionally, its transparent billing tools and ready-to-use documentation reduce administrative burdens while maximizing reimbursements for care management services.
FAQs
How does between-visit care help manage chronic conditions and prevent hospitalizations?
Between-visit care focuses on managing chronic conditions by addressing potential risks early, keeping an eye on symptoms, and ensuring patients adhere to their treatment plans. Services like Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Transitional Care Management (TCM) empower healthcare providers to take proactive steps, which can reduce complications and prevent unnecessary hospitalizations.
By streamlining care coordination and fostering consistent patient engagement, these programs improve symptom control, encourage medication adherence, and promote better health outcomes. This proactive approach not only elevates the standard of care but also helps minimize emergency visits and acute health crises, benefiting both patients and providers from clinical and financial perspectives.
How does Remote Patient Monitoring help reduce hospital readmissions?
Remote Patient Monitoring (RPM) significantly helps in lowering hospital readmissions by enabling proactive healthcare management. By continuously monitoring vital signs and other critical health metrics, RPM can detect early warning signs of potential health issues. This empowers care teams to act quickly, addressing concerns before they escalate into more serious conditions.
Additionally, RPM enhances the development of personalized care plans by providing real-time data. This ensures that patients receive customized guidance and support tailored to their specific needs. These timely interventions not only lead to better health outcomes for patients but also reduce the reliance on emergency room visits or hospital admissions, streamlining healthcare delivery and improving overall efficiency.
What are the best ways for healthcare practices to implement between-visit care models effectively?
Healthcare practices can effectively adopt between-visit care models by concentrating on clear protocols, efficient communication, and active patient involvement. Begin by creating structured workflows for care coordination, ensuring every team member understands their specific roles and responsibilities. Incorporating technology, such as real-time monitoring tools, allows you to keep track of patient health and address potential risks early.
Equally important is emphasizing post-discharge follow-ups and routine check-ins to sustain consistent care. By using accessible platforms or apps, you can encourage patients to take an active role in managing their care plans. These measures not only enhance patient outcomes but also help lower the chances of avoidable hospital admissions and emergency visits.
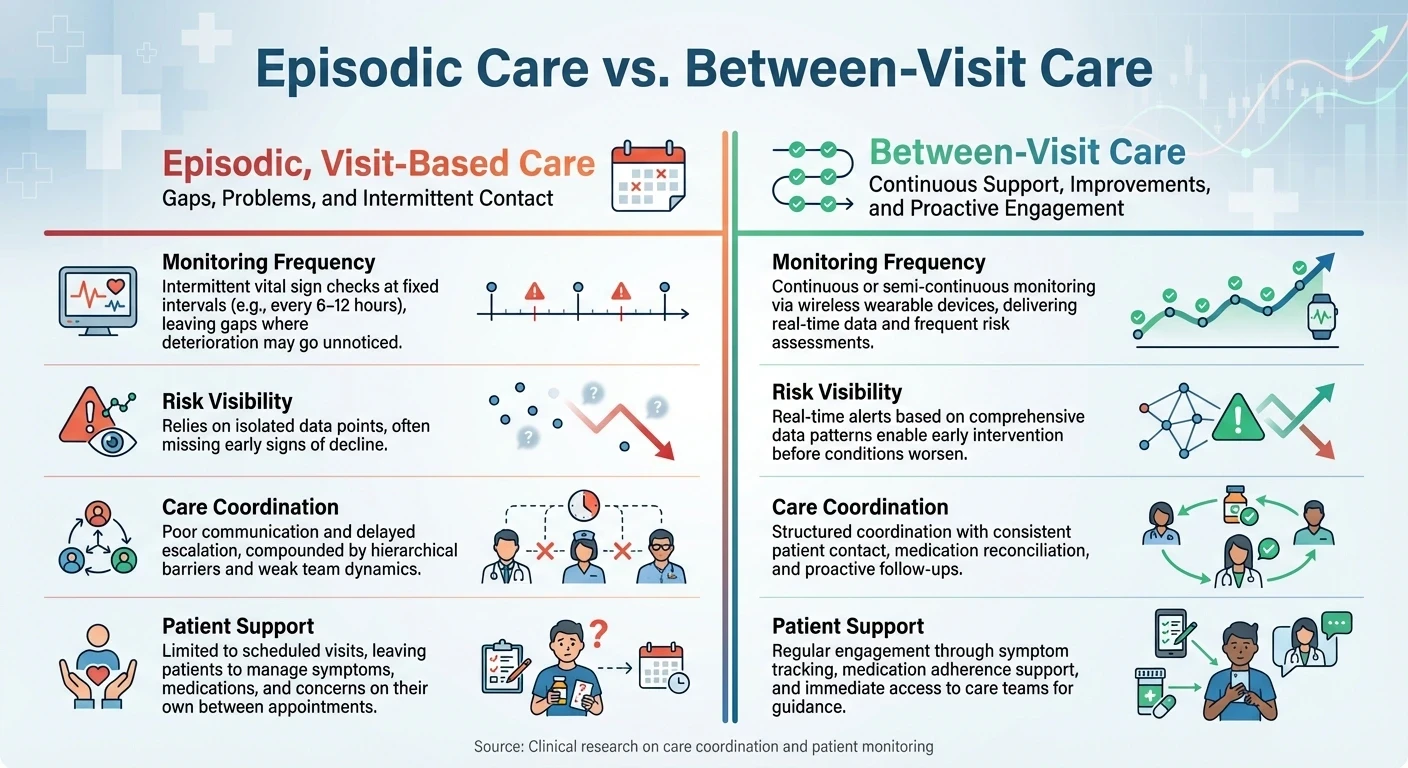
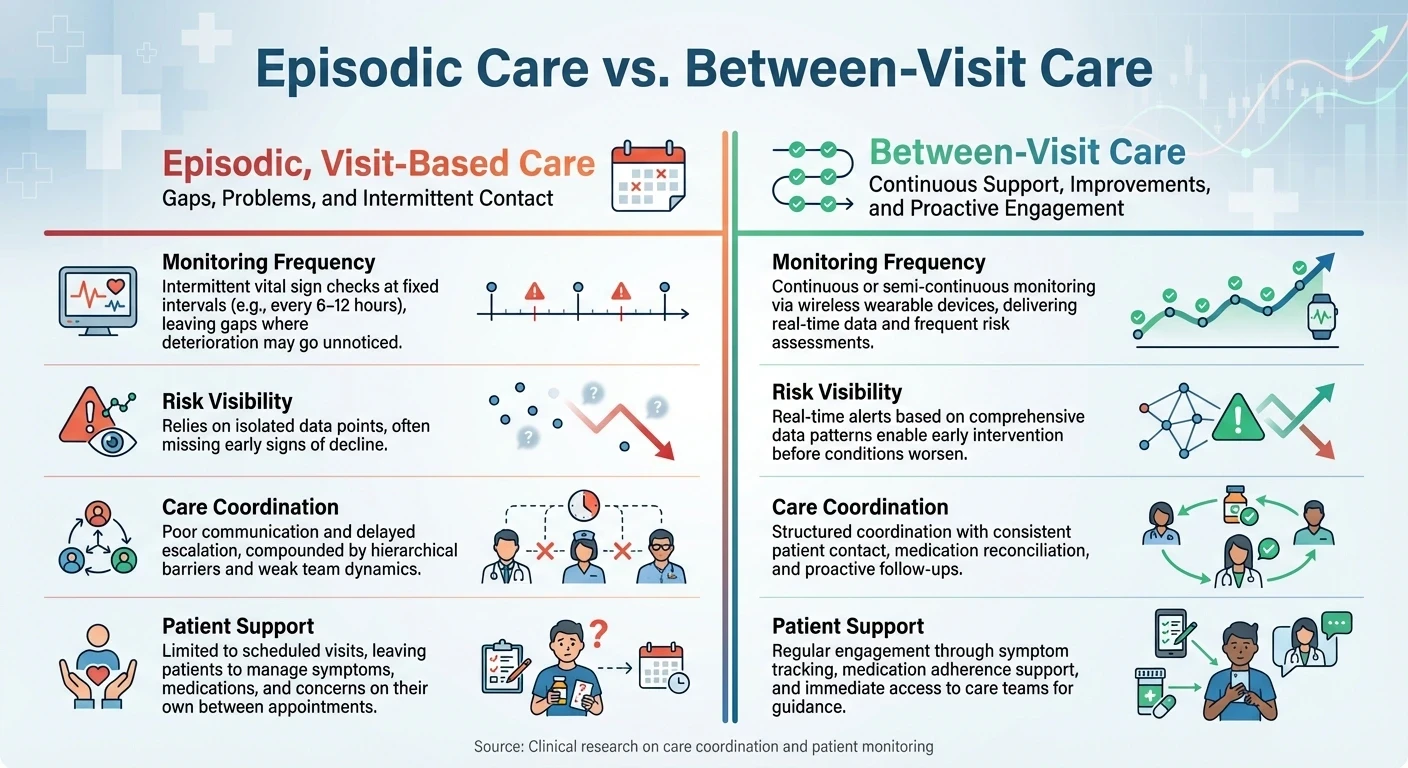
Episodic Care vs Between-Visit Care: Key Differences in Patient Monitoring
The traditional visit-based care model has inherent blind spots when it comes to monitoring patients, particularly those with chronic conditions. These gaps leave extended periods where a patient’s health can decline unnoticed, often resulting in emergency room visits or hospitalizations. Office visits alone cannot meet the ongoing needs of patients who require consistent attention and coordination. This highlights the importance of proactive, continuous monitoring strategies.
Problems with Episodic, Visit-Based Care
A significant drawback of visit-based care is its fragmented oversight. Patients with chronic conditions frequently see multiple specialists, but poor coordination among providers means no one has a complete view of the patient’s overall health. This lack of integration often results in medication conflicts, redundant procedures, and missed opportunities to address worsening conditions before they become critical.
Intermittent monitoring is another shortfall, as it creates periods where health deterioration can go unnoticed. Research indicates that protocols for recording vital signs are often not followed consistently. For example, the National Early Warning Score 2 (NEWS2) is frequently underestimated, with accurate assessments revealing a higher risk level in 27% of cases.
Additionally, delayed escalation is a recurring issue. Timely interventions are undermined, with full adherence to escalation protocols observed in only 8% of serious adverse events. Monitoring delays occurred in 81% of cases, and appropriate escalation for elevated early warning scores was implemented in just 60% of moderate-risk cases and 41% of high-risk cases. Even among patients with the highest risk scores, only half were reviewed by senior staff or a Medical Emergency Team. High patient volumes and the perception that moderately elevated scores wouldn’t change management often deter nurses from notifying physicians.
Additionally, delayed escalation is a recurring issue. Timely interventions are undermined, with full adherence to escalation protocols observed in only 8% of serious adverse events. Monitoring delays occurred in 81% of cases, and appropriate escalation for elevated early warning scores was implemented in just 60% of moderate-risk cases and 41% of high-risk cases. Even among patients with the highest risk scores, only half were reviewed by senior staff or a Medical Emergency Team. High patient volumes and the perception that moderately elevated scores wouldn’t change management often deter nurses from notifying physicians.
Episodic Care vs. Between-Visit Care
Continuous care offers clear advantages over episodic, visit-based models. The following table highlights key differences and demonstrates how between-visit care addresses the shortcomings of traditional approaches:
Aspect | Episodic, Visit-Based Care | Between-Visit Care |
|---|---|---|
Monitoring Frequency | Intermittent vital sign checks at fixed intervals (e.g., every 6–12 hours), leaving gaps where deterioration may go unnoticed | Continuous or semi-continuous monitoring via wireless wearable devices, delivering real-time data and frequent risk assessments |
Risk Visibility | Relies on isolated data points, often missing early signs of decline | Real-time alerts based on comprehensive data patterns enable early intervention before conditions worsen |
Care Coordination | Poor communication and delayed escalation, compounded by hierarchical barriers and weak team dynamics | Structured coordination with consistent patient contact, medication reconciliation, and proactive follow-ups |
Patient Support | Limited to scheduled visits, leaving patients to manage symptoms, medications, and concerns on their own between appointments | Regular engagement through symptom tracking, medication adherence support, and immediate access to care teams for guidance |
Recognizing these gaps is a critical step toward adopting more effective care models that prioritize continuous monitoring and patient-centered solutions.
Using CCM, RPM, and TCM to Reduce Hospitalizations
Integrating Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Transitional Care Management (TCM) into between-visit care programs can help identify early warning signs before emergencies occur. CCM lays the groundwork with ongoing care coordination, RPM provides real-time tracking of patient vitals, and TCM ensures smooth transitions after hospital discharge. Together, these programs work as a cohesive system to address gaps that often lead to preventable hospitalizations.
Chronic Care Management (CCM): Establishing the Framework
CCM provides a structured approach to managing patients with two or more chronic conditions expected to persist for at least 12 months. This program extends care beyond the clinic, focusing on medication reviews, personalized care plans, and proactive patient outreach. Care teams use comprehensive risk assessments, evaluating factors like social support and medication adherence, to identify patients most at risk for hospitalization.
Core elements of CCM include clear medication schedules, shared treatment plans, and self-management education. This is especially critical given that approximately two-thirds of Medicare beneficiaries manage multiple chronic conditions. Multidisciplinary teams customize care by integrating behavioral health into primary care settings and employing social work teams to address social determinants of health. These strategies significantly lower the likelihood of hospitalizations.
This foundational framework is further strengthened by RPM, which enables continuous tracking of patient health metrics.
Remote Patient Monitoring (RPM): Detecting Issues Early
RPM revolutionizes care by enabling real-time monitoring of patient vitals through connected devices such as blood pressure monitors and glucose meters. These devices transmit data directly to care teams, allowing them to identify trends and intervene early, often before complications arise. This approach is particularly beneficial for high-risk patients, including those recently discharged or those struggling with poorly managed chronic conditions.
For instance, a program monitoring patients with chronic heart disease through daily RPM saw a 37% reduction in hospital readmissions. Similarly, diabetes patients who received regular RPM reminders for submitting blood sugar levels and insulin usage achieved better glycemic control and fewer emergency room visits due to diabetic complications. Across various conditions, RPM has been shown to reduce hospital admissions, shorten hospital stays, and decrease emergency department visits in nearly 50% of studies, with significant results for chronic obstructive pulmonary disease (COPD).
While RPM provides continuous oversight, TCM ensures that patients transition safely back to their communities after hospital stays.
Transitional Care Management (TCM): Ensuring Smooth Transitions
TCM addresses the critical first 30 days after hospital discharge, a period when patients are highly vulnerable to readmission. Through structured workflows, including initial outreach, medication reconciliation, and timely follow-ups, TCM ensures continuity of care. This comprehensive support helps bridge communication gaps between hospital and primary care teams, reducing risks like medication errors, missed appointments, and rapid health declines.
Accountable Care Organizations (ACOs) that implement strong TCM programs often achieve 20-30% reductions in 30-day readmissions, along with fewer emergency department visits. The program also strengthens communication between providers and ensures patients receive clear discharge instructions. Together, CCM, RPM, and TCM form an integrated care continuum that reduces hospital readmissions and enhances patient outcomes.
Building Scalable Between-Visit Care with OnCare360
OnCare360 builds on the principles of continuous care coordination and real-time monitoring, offering a platform designed to scale efficiently. Managing Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Transitional Care Management (TCM) requires a robust operational framework to handle ongoing monitoring, documentation, compliance, and care coordination. OnCare360 delivers this through a unified system tailored for physician groups and value-based organizations that care for high-risk chronic patients between clinic visits. By combining AI-driven workflow automation with certified care teams and medical-grade monitoring devices, the platform reduces operational strain while maintaining clinical quality and audit readiness. Below, we explore how OnCare360's integrated features support scalable and compliant care delivery.
Unified Care Management Platform
OnCare360 consolidates key care management functions - including CCM, RPM, TCM, and behavioral health - into a single, streamlined workflow. This eliminates the inefficiencies of fragmented systems by enabling care teams to work within one platform that handles patient enrollment, care plan execution, medication reconciliation, vital sign monitoring, and billing documentation in real time. By centralizing these functions, the platform minimizes missed interventions and redundant efforts, reinforcing the continuous care model essential for reducing preventable hospitalizations.
The platform also incorporates cellular medical-grade devices that automatically transmit vital signs without requiring any setup by patients. These devices feed data directly into the care coordination system, allowing clinical teams to monitor high-risk patients consistently and intervene before complications arise. For practices managing large populations of patients with chronic conditions, this infrastructure removes technical barriers to RPM adoption and ensures a steady flow of data, regardless of patients' familiarity with technology.
AI-Driven Risk Prioritization and Monitoring
OnCare360 leverages AI-powered care coordination to identify risk signals, prioritize tasks, and provide documentation suggestions - all while keeping licensed clinicians in full control of care decisions and interventions. The system analyzes incoming vital signs, flags concerning trends, and routes alerts to care coordinators based on established clinical protocols and patient acuity levels. This approach enables small care teams to efficiently manage large patient populations without compromising clinical oversight or quality.
The AI system also automates routine tasks such as logging communications, updating care plans, and tracking billing time. This allows care coordinators to focus on patient engagement and timely interventions while maintaining the documentation standards necessary for audits and reducing the risk of clawbacks. By balancing automation with clinical oversight, OnCare360 ensures that care teams can manage growing patient panels effectively while maintaining high standards of care.
Scalability and Compliance for Value-Based Care
OnCare360 is designed to scale seamlessly across specialties such as primary care, cardiology, nephrology, and endocrinology, without requiring extensive customizations or IT overhauls. The cloud-based platform integrates with existing EHR systems, enabling quick deployment across multi-site organizations. Practices can start with a small pilot group and gradually expand as they demonstrate improvements in patient engagement, vital sign stability, and reductions in acute care episodes.
The platform also includes robust enrollment safeguards and eligibility checks, ensuring that billing aligns with clinical criteria rather than aggressive enrollment strategies. Monthly billing reports, denial management support, and clear documentation summaries simplify administrative tasks for practice managers and revenue cycle management (RCM) teams, improving clean-claim rates. For organizations involved in TEAM, ACCESS, or other value-based payment programs, OnCare360 provides the tools needed for continuous monitoring, care gap closure, and outcome tracking - key elements for success in shared savings and risk-adjusted payment models.
Measuring Outcomes and ROI from Between-Visit Care
To truly understand the value of continuous between-visit care, it's essential to evaluate both patient outcomes and financial returns. This requires analyzing lagging indicators, such as hospitalizations and emergency department visits, alongside leading indicators that help identify emerging risks early.
Key Metrics for Reducing Preventable Hospitalizations
Metrics like all-cause hospitalization and emergency department visit rates are critical in assessing whether between-visit care helps prevent avoidable admissions. However, relying solely on 30-day readmission rates can be misleading, as some acute care returns are reclassified during this period.
A more thorough evaluation includes financial and process metrics that reflect overall care costs and early warning signs of health deterioration. Establishing baseline metrics before implementing a program is vital for tracking improvements over time.
Real-world examples highlight the effectiveness of between-visit care. In 2023, Medicare Advantage patients in Humana's value-based care arrangements experienced 32.1% fewer inpatient hospital admissions and 11.6% fewer emergency department visits compared to those in non–value-based care models. Similarly, a 2024 study by the VillageMD Research Institute revealed that patients who maintained regular engagement with their primary care providers saw lower hospital admission rates. In contrast, patients with chronic conditions like COPD and congestive heart failure who had fewer visits experienced an increase in admissions.
"Our report paints a clear picture: value-based practices deliver better patient experiences and health outcomes. Patients spend more time with their primary care clinician, which means more preventive care and better management of chronic diseases, like diabetes and high blood pressure. Seniors in value-based care models receive the care they deserve with a clinician who holistically understands their care needs." - Kate Goodrich, MD, MHS, Chief Medical Officer, Humana
Beyond clinical improvements, it's equally important to measure the financial and operational impact of between-visit care.
Calculating Financial and Clinical ROI
Once outcomes are measured, calculating return on investment (ROI) helps validate the financial viability of between-visit care programs. This involves comparing revenue gains and cost reductions against the total program investment. A good starting point is establishing baseline data, such as average administrative time per patient, revenue generated from care management billing codes, and costs related to missed appointments.
Direct financial benefits include increased reimbursements from care management billing codes and revenue recovery from fewer no-shows. Patient engagement platforms can reduce no-show rates by 20–40%, a significant improvement considering that no-shows account for 15–30% of lost revenue in small practices. For instance, a practice generating $500,000 annually with a 20% no-show rate could recover approximately $30,000 each year by improving appointment adherence.
Indirect benefits also play a major role, particularly in reducing acute care utilization. Chronic conditions drive 85% of total healthcare costs, making their management a key financial consideration. Additionally, evaluating the broader value on investment (VOI) - including enhanced patient experience, improved clinical outcomes, and increased care team satisfaction - provides a more comprehensive view of long-term program sustainability, even when these benefits aren't immediately visible in financial statements.
Common ROI pitfalls include overlooking indirect costs, overestimating patient engagement levels, and failing to account for quality improvements. Accurate ROI assessments should consider the shift from volume-based to value-based care and the cumulative benefits of sustained patient engagement. Practices using robust patient engagement platforms report a 3-year ROI ranging from 6:1 to 15:1, along with reduced administrative costs and improved patient retention.
Conclusion: Reducing Hospitalizations with OnCare360
Preventable hospitalizations not only strain resources but also disrupt the continuity of patient care. Between-visit care programs have demonstrated their ability to lower such admissions, enhance chronic disease management, and increase patient satisfaction. However, many healthcare practices face challenges like fragmented tools, inconsistent processes, and the operational difficulties of scaling these programs effectively.
OnCare360 addresses these hurdles by offering a streamlined platform that integrates care coordination, AI-powered prioritization, and medical-grade home monitoring. This unified system eliminates the inefficiencies caused by disconnected tools, which often lead to gaps in care transitions. Certified care coordinators, supported by standardized pathways and real-time patient data, enable practices to proactively identify high-risk patients and intervene before conditions escalate.
The platform's AI-driven automation, combined with clinical oversight, allows small teams to manage larger patient populations while maintaining audit-ready documentation. Its cellular medical-grade devices simplify patient engagement, providing continuous monitoring of vital signs without requiring Wi-Fi or complex setups. This seamless flow of real-time data enhances communication across care settings, ensures timely medication reconciliation, and strengthens patient safety - all critical components of effective care continuity. These operational improvements align directly with the goals of value-based care.
For physician groups and organizations focused on value-based models, OnCare360 delivers measurable improvements across clinical, operational, and financial domains. By optimizing care workflows and reducing emergency visits, the platform supports the shift toward value-based care. Additionally, its transparent billing tools and ready-to-use documentation reduce administrative burdens while maximizing reimbursements for care management services.
FAQs
How does between-visit care help manage chronic conditions and prevent hospitalizations?
Between-visit care focuses on managing chronic conditions by addressing potential risks early, keeping an eye on symptoms, and ensuring patients adhere to their treatment plans. Services like Chronic Care Management (CCM), Remote Patient Monitoring (RPM), and Transitional Care Management (TCM) empower healthcare providers to take proactive steps, which can reduce complications and prevent unnecessary hospitalizations.
By streamlining care coordination and fostering consistent patient engagement, these programs improve symptom control, encourage medication adherence, and promote better health outcomes. This proactive approach not only elevates the standard of care but also helps minimize emergency visits and acute health crises, benefiting both patients and providers from clinical and financial perspectives.
How does Remote Patient Monitoring help reduce hospital readmissions?
Remote Patient Monitoring (RPM) significantly helps in lowering hospital readmissions by enabling proactive healthcare management. By continuously monitoring vital signs and other critical health metrics, RPM can detect early warning signs of potential health issues. This empowers care teams to act quickly, addressing concerns before they escalate into more serious conditions.
Additionally, RPM enhances the development of personalized care plans by providing real-time data. This ensures that patients receive customized guidance and support tailored to their specific needs. These timely interventions not only lead to better health outcomes for patients but also reduce the reliance on emergency room visits or hospital admissions, streamlining healthcare delivery and improving overall efficiency.
What are the best ways for healthcare practices to implement between-visit care models effectively?
Healthcare practices can effectively adopt between-visit care models by concentrating on clear protocols, efficient communication, and active patient involvement. Begin by creating structured workflows for care coordination, ensuring every team member understands their specific roles and responsibilities. Incorporating technology, such as real-time monitoring tools, allows you to keep track of patient health and address potential risks early.
Equally important is emphasizing post-discharge follow-ups and routine check-ins to sustain consistent care. By using accessible platforms or apps, you can encourage patients to take an active role in managing their care plans. These measures not only enhance patient outcomes but also help lower the chances of avoidable hospital admissions and emergency visits.

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?


