The Rise of Between-Visit Care in 2026: What Practices Must Know





OnCare360
Nov 2, 2025
Between-visit care, or longitudinal care management, focuses on supporting patients outside traditional office visits. It addresses gaps in chronic disease management, behavioral health, and post-acute care by using coordinated teams and technology. With 90% of U.S. healthcare spending tied to chronic and mental health conditions, this shift is critical for improved outcomes and financial sustainability.
Physician groups, practice administrators, and value-based care leaders face operational challenges in adapting to this model, including compliance with CMS updates, reimbursement changes, and workflow integration. This article outlines actionable steps to implement Chronic Care Management (CCM), Remote Patient Monitoring (RPM), Behavioral Health Integration (BHI), and Transitional Care Management (TCM) programs effectively. Readers will gain insights into policy updates, AI-driven tools, and strategies to align care delivery with value-based models while maintaining audit readiness.
Key takeaways include:
How to optimize care coordination workflows for compliance and efficiency.
Navigating 2026 CMS reimbursement updates for CCM, RPM, BHI, and TCM.
Leveraging AI and unified platforms to scale between-visit care.
Key Models of Between-Visit Care
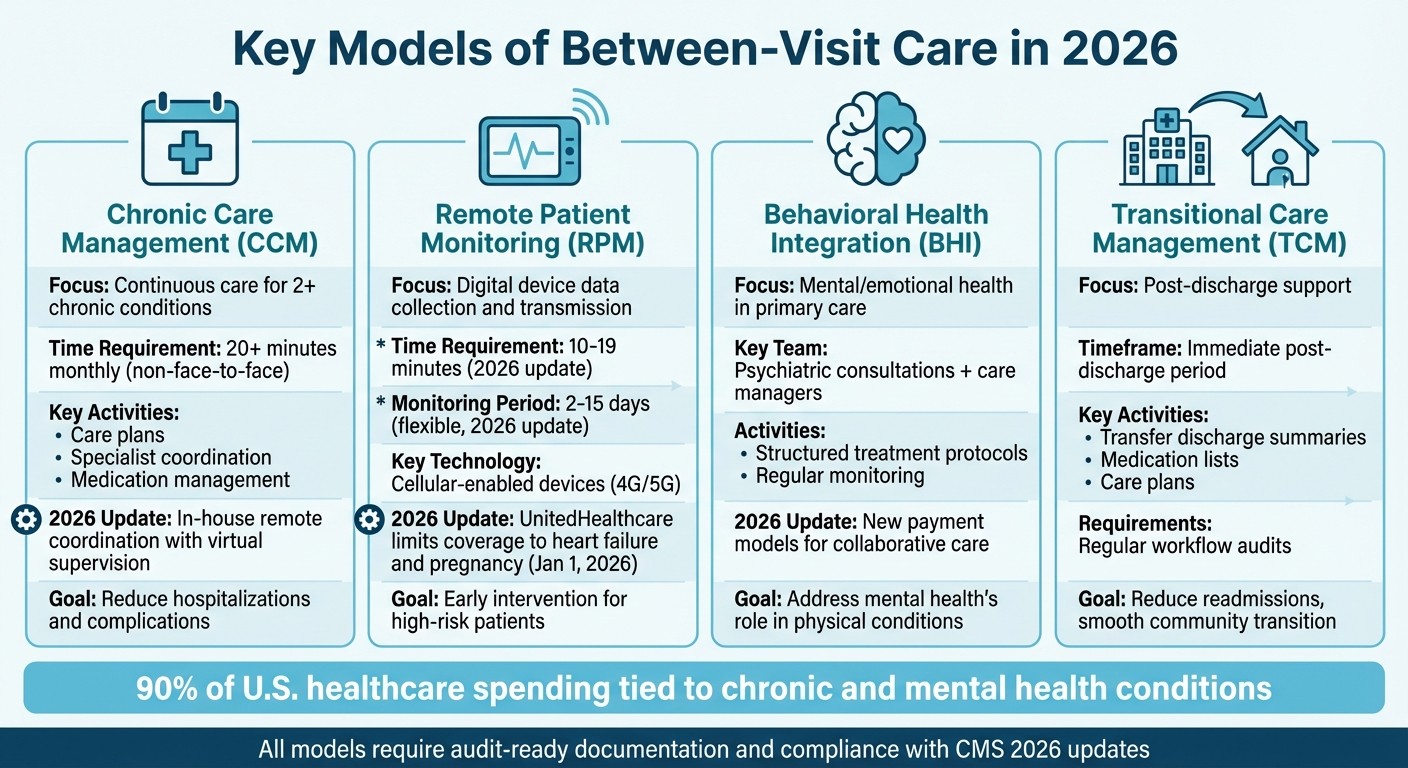
Four Key Between-Visit Care Models: CCM, RPM, BHI, and TCM Comparison 2026
Between-visit care includes several distinct approaches designed to meet specific patient needs. The primary models - Chronic Care Management (CCM), Remote Patient Monitoring (RPM), Behavioral Health Integration (BHI), and Transitional Care Management (TCM) - each have unique eligibility criteria, reimbursement structures, and compliance requirements. These models collectively highlight the ongoing evolution in healthcare as we approach 2026.
Chronic Care Management (CCM)
CCM focuses on providing continuous, proactive care for patients managing two or more chronic conditions. Unlike episodic care, CCM emphasizes activities that happen between office visits, such as creating comprehensive care plans, coordinating with specialists, and managing medications. These efforts aim to reduce complications and prevent hospitalizations.
Looking ahead to 2026, practices must ensure compliance with updated CMS eligibility criteria and maintain thorough documentation. CCM requires tracking at least 20 minutes of non–face-to-face care monthly, along with detailed records of all care coordination efforts. The latest updates encourage practices to adopt in-house remote care coordination with virtual supervision, enabling clinical teams to manage shorter, more frequent interactions effectively. This approach not only supports compliance but also helps improve long-term patient outcomes by reducing hospitalizations.
Remote Patient Monitoring (RPM)
RPM uses digital devices to collect and transmit physiological data, enabling early intervention and ongoing health monitoring. Cellular-enabled devices are a standout feature, as they reduce IT challenges by avoiding reliance on Wi-Fi connections. This continuous monitoring is particularly valuable for high-risk patients, allowing for timely responses and better health outcomes.
The 2026 CMS updates introduce new CPT codes to accommodate flexible monitoring periods (ranging from 2 to 15 days) and shorter interaction requirements (10 to 19 minutes). Additionally, UnitedHealthcare will limit RPM coverage to conditions like heart failure and pregnancy starting January 1, 2026. Practices must carefully review updated guidelines from CMS and commercial payors to ensure patient eligibility and compliance.
Behavioral Health Integration (BHI)
BHI brings mental and emotional health services into primary care, acknowledging the critical role mental health plays in managing physical conditions such as diabetes or heart disease. Behavioral health remains a leading area for telehealth, and the 2026 updates include new payment models to support collaborative care.
For successful implementation, practices must establish clear roles within virtual care teams to minimize confusion and ensure compliance. BHI programs typically involve regular psychiatric consultations, care manager support, and structured treatment protocols. Consistent documentation and monitoring are essential for maintaining program effectiveness and meeting compliance requirements.
Transitional Care Management (TCM)
TCM is designed to support patients immediately after discharge from a hospital or care facility, with the goal of reducing readmissions and ensuring a smooth transition to community-based care. This time-sensitive program focuses on the critical post-discharge period, emphasizing the seamless transfer of discharge summaries, medication lists, and care plans. Regular audits of workflows can help practices identify inefficiencies and address compliance concerns.
Key takeaways for 2026:
CCM emphasizes ongoing, coordinated care for patients with multiple chronic conditions, with a focus on continuity and compliance.
RPM utilizes cellular devices for continuous health monitoring, though coverage restrictions are tightening under some commercial insurers.
BHI integrates mental health into primary care, supported by updated payment models for collaborative care.
TCM provides focused, short-term support after hospital discharge to prevent readmissions and ensure effective transitions back to the community.
2026 Policy and Reimbursement Changes
As healthcare continues to shift toward between-visit care, staying informed about policy updates becomes essential for maintaining efficient operations. The Calendar Year 2026 Medicare Physician Fee Schedule (PFS) Final Rule, effective January 1, 2026, introduces reimbursement changes that directly impact Chronic Care Management (CCM), Remote Patient Monitoring (RPM), Behavioral Health Integration (BHI), and Transitional Care Management (TCM). For participants in qualifying Alternative Payment Models (APMs), the conversion factor increases to $33.57, while non-qualifying participants will see a slightly lower rate of $33.40. These adjustments will shape billing practices and bring heightened regulatory oversight.
CMS Reimbursement Updates
The 2026 PFS includes new RPM codes designed to address shorter monitoring periods (2 to 15 days) and reduced management times (10 to 20 minutes). These updates allow for more frequent billing, provided workflows are adjusted and documentation remains precise. However, overall payment increases are tempered by other changes, such as a -2.5% reduction in specific areas.
Compliance and Audit Requirements
CMS is increasing its focus on Medicare provider enrollment, introducing additional grounds for retroactive revocations and deactivations [8]. This heightened scrutiny means even minor documentation mistakes could trigger audits. Practices must prioritize maintaining audit-ready documentation to safeguard their billing and enrollment processes.
Value-Based Care Incentives
Alongside stricter compliance measures, CMS is updating quality measure incentives. For 2026, the Merit-based Incentive Payment System (MIPS) will feature 5 new quality measures and 3 new improvement activities, while 10 outdated measures and 8 activities will be removed. Practices focusing on chronic disease management, care coordination, and patient engagement can enhance their MIPS scores. These updates emphasize the importance of delivering consistent, patient-centered care that extends beyond the traditional office visit.
Technology for Scaling Between-Visit Care
Expanding between-visit care requires technology that simplifies workflows, reduces administrative tasks, and delivers actionable insights - all without overwhelming smaller clinical teams. Unified platforms serve as central hubs, seamlessly connecting electronic health records (EHRs), virtual care tools, health monitoring devices, and online pharmacy or lab portals into a single, streamlined system. By integrating these tools, healthcare teams can overcome fragmented systems and focus on delivering proactive, coordinated care. This technological foundation supports the development of more connected and efficient care solutions.
Unified Platforms for Workflow Integration
Fragmented systems often lead to duplicated efforts, missed follow-ups, and inconsistent care tracking. To ensure continuous, effective care, a unified system is crucial. These platforms bring together various programs into a single, cohesive workflow, reducing inefficiencies and enabling care teams to manage large patient populations more effectively. For example, OnCare360 integrates chronic care management, remote monitoring, transitional care, behavioral health services, medication reconciliation, and care gap tracking into one interface. This consolidation allows care teams to access patient histories, monitor interventions, and maintain audit-ready documentation - all without toggling between multiple systems or manually merging data. With unified workflows in place, advanced analytics can further enhance decision-making and care delivery.
AI-Driven Care Coordination
AI is reshaping between-visit care by analyzing patient data patterns, identifying potential health risks, and offering tailored care recommendations. In remote patient monitoring, AI-based platforms integrate with EHRs to provide real-time insights, automate routine tasks, generate structured notes, and streamline billing processes. This creates a collaborative model where AI highlights priorities, flags risks, and suggests documentation cues, while clinicians retain control over final decisions and care interventions. By reducing manual documentation and missed opportunities, this approach enables small clinical teams to efficiently manage larger patient panels.
Cellular Devices for Patient Monitoring
Consistent data transmission is essential for remote patient monitoring, particularly for patients in rural areas or those without reliable Wi-Fi. To address this, RPM systems must support various connectivity options, such as cellular (4G/5G) and Bluetooth, ensuring uninterrupted data flow regardless of location. Cellular-enabled devices simplify the process by eliminating technical barriers like app downloads, password resets, or home network configurations. These medical-grade devices integrate directly into care platforms, providing continuous monitoring for high-risk patients. This setup not only minimizes IT challenges but also facilitates earlier interventions, leading to improved patient outcomes.
Implementation Steps for Physician Practices
To successfully implement between-visit care, physician practices must align their patients' needs with compliant workflows and measurable outcomes. This involves assessing patient populations, creating detailed, audit-ready processes, and monitoring both clinical improvements and financial returns. The ultimate aim is to establish a program that grows sustainably without overloading staff or increasing compliance risks. These steps build on previously discussed care models to create a scalable and effective system for between-visit care.
Evaluating Patient Panels and Needs
Start by identifying care gaps, such as missed screenings, treatments, or follow-ups. Patients with multiple chronic conditions are particularly vulnerable to these gaps. For instance, medication non-adherence alone is linked to 125,000 deaths annually, with nearly 50% of chronic disease patients discontinuing medication refills within the first year of diagnosis.
Health Risk Assessments (HRAs), conducted during Annual Wellness Visits (AWVs), are invaluable tools for pinpointing patients who require between-visit support. These assessments can uncover missed opportunities for preventive care, such as pneumonia vaccinations, colorectal screenings, and mammograms. Beyond medical needs, practices should address social determinants of health by connecting patients to resources like pharmaceutical discounts, transportation services, food banks, and utility assistance. Programs like Chronic Care Management (CCM) provide dedicated care teams to maintain regular contact with patients, address real-time challenges, and coordinate care across both medical and social domains.
Creating Compliant Workflows
The CMS ACCESS Model, set to begin on July 1, 2026, represents a shift in Medicare reimbursement from fee-for-service to Outcome-Aligned Payments (OAPs), which reward practices for achieving measurable health outcomes. This model complements technology-driven solutions that streamline care delivery. To align with these changes, practices must develop workflows that can track and demonstrate clinical improvements, such as reducing blood pressure by 10 mmHg. Key performance metrics include condition-specific biomarkers like HbA1c, blood pressure, lipids, and weight, alongside Patient Reported Outcome Measures (PROMs) that assess pain, mood, and overall function.
Automating key processes - such as communication logs, time tracking, care plan documentation, and eligibility checks - ensures efficient and accurate documentation. Every patient interaction should include clear consent processes and meet audit-ready standards. Since ACCESS Model payments will be tied to the percentage of patients meeting defined outcome targets, precise documentation and outcome tracking are essential for optimizing revenue.
Tracking Outcomes and ROI
To validate the effectiveness of between-visit care, practices need to measure outcomes that demonstrate both clinical progress and financial returns. Key metrics include engagement rates, medication adherence, stability of vital signs, timeliness of interventions, reduced no-show rates, and fewer emergency department visits or acute care episodes. Additionally, tracking the revenue generated from CCM, RPM, and TCM services - as well as cost savings from reduced hospitalizations and improved chronic disease management - is crucial.
Real-time dashboards can help practices monitor monthly performance across patient panels. These tools allow teams to identify which interventions are achieving the best results and where workflows may need refinement. Sharing these insights with clinical staff, administrators, and payors highlights the tangible benefits of between-visit care. This transparency also positions practices to succeed in shared savings programs, capitation arrangements, and hybrid payment models as value-based care continues to expand.
Conclusion: Preparing for Between-Visit Care in 2026
This guide has highlighted the growing importance of proactive, between-visit care in reshaping practice operations. For physician practices aiming to excel within value-based care models, this shift is no longer optional. By 2026, CMS quality reporting will emphasize coordinated, patient-focused care that extends beyond traditional office visits. Practices will need to demonstrate measurable outcomes and consistent follow-through to align with these evolving standards. Those that embrace care beyond the clinic will be better equipped to thrive under CMS's redefined approach to value.
Technology plays a critical role in addressing these demands. Advanced care models driven by technology provide the tools needed for audit-ready documentation and compliance with CMS requirements. Practices that achieve strong compliance performance will benefit from fewer claim denials, more efficient audits, and operational improvements, which can lead to increased market share and profitability. Additionally, policymakers are expanding incentives tied to alternative payment models, linking reimbursement directly to outcomes and making technology indispensable for tracking and demonstrating progress.
To capitalize on these advancements, practices should adopt scalable workflows that meet compliance standards while enabling revenue capture from CCM, RPM, and TCM services. Integrating AI-powered care coordination, cellular monitoring devices, and robust documentation systems can ease operational challenges while enhancing clinical outcomes. These tools contribute to better management of chronic conditions, improved patient engagement, and stronger financial performance.
The time to act is now. Practices must assess their patient panels, close care gaps, implement compliant processes, and track measurable outcomes to secure revenue and maintain a competitive edge. Delaying these steps risks falling behind as CMS continues shifting reimbursement toward longitudinal, home-centered care models. By investing in the right infrastructure, physician groups can achieve better patient outcomes, reduced avoidable costs, and a stronger competitive position in the rapidly changing healthcare environment.
FAQs
What are the main benefits of between-visit care for managing chronic conditions?
Between-visit care plays a key role in managing chronic diseases by prioritizing consistent monitoring and timely interventions. This proactive approach helps patients avoid unnecessary emergency room visits and hospital admissions, contributing to better overall health outcomes. It also strengthens medication adherence and ensures smoother collaboration among healthcare providers, enhancing care coordination.
Another advantage is its ability to boost patient engagement. By involving patients more actively in their care, it fosters a sense of ownership and leads to improved long-term health results. For healthcare practices, between-visit care aligns seamlessly with value-based care objectives, supporting cost efficiency and enhancing financial performance.
What steps should practices take to stay compliant with CMS updates for between-visit care in 2026?
To align with the 2026 CMS updates, practices need to embrace integrated technology solutions that simplify compliance tasks. This includes automating documentation, monitoring care activities, and ensuring service requirements are consistently validated. Accurate record-keeping and smooth care transitions are essential to meet the new standards effectively.
Equally important is ongoing staff training on updated policies. Leveraging real-time audit tools and meticulously documenting every patient interaction can help practices stay on track with CMS guidelines. These measures not only support compliance but also enhance patient care, reinforcing the principles of value-based care.
How does technology help healthcare practices enhance between-visit care?
Technology plays a crucial role in transforming between-visit care by simplifying communication, enhancing care coordination, and supporting remote monitoring and telehealth services. It enables healthcare practices to exchange data effortlessly, automate repetitive tasks, and align workflows, ultimately making care delivery more efficient and focused on the patient.
Using tools such as remote patient monitoring (RPM), chronic care management (CCM), and behavioral health integration (BHI), healthcare teams can maintain consistent engagement with patients between visits. These tools help identify potential health concerns early and facilitate timely interventions. The result is not only improved patient outcomes but also greater operational efficiency and stronger financial performance within value-based care frameworks.
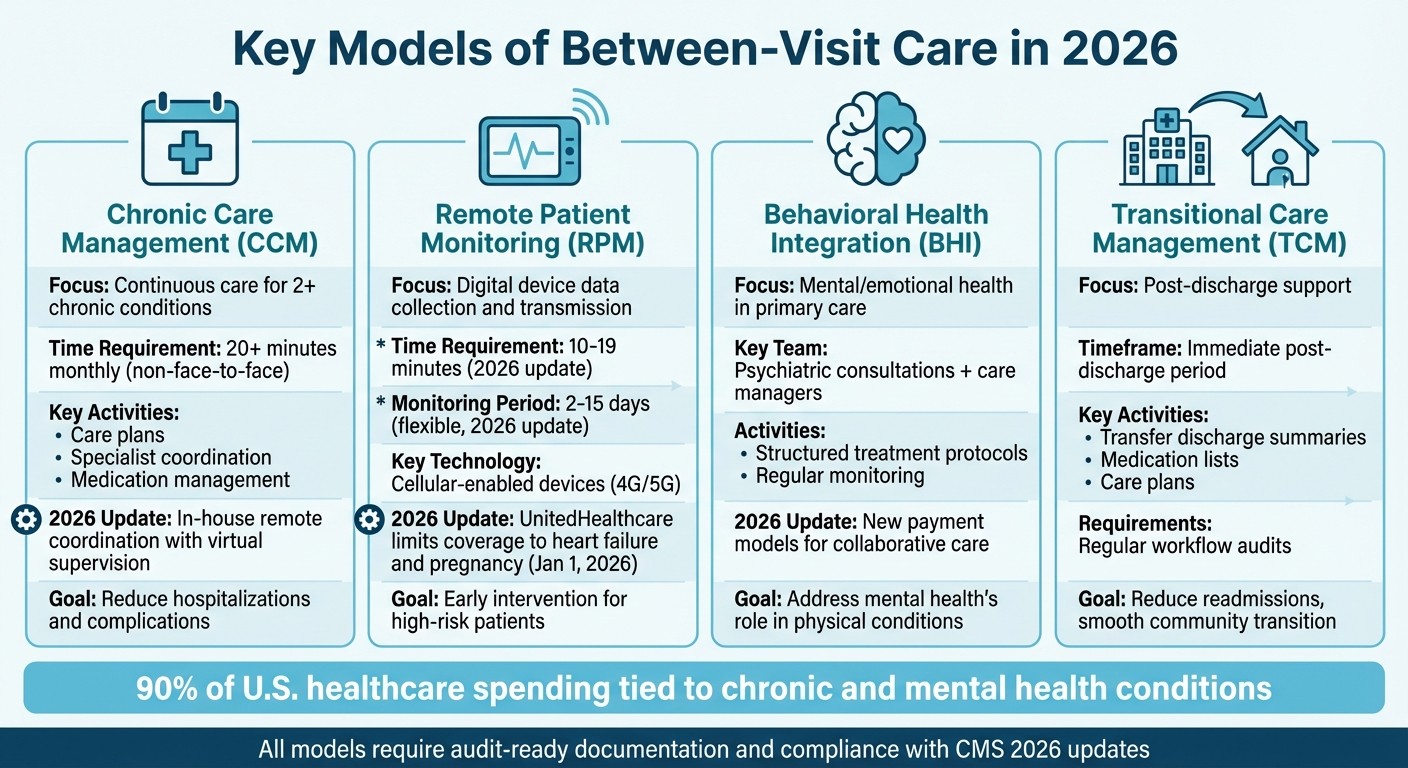
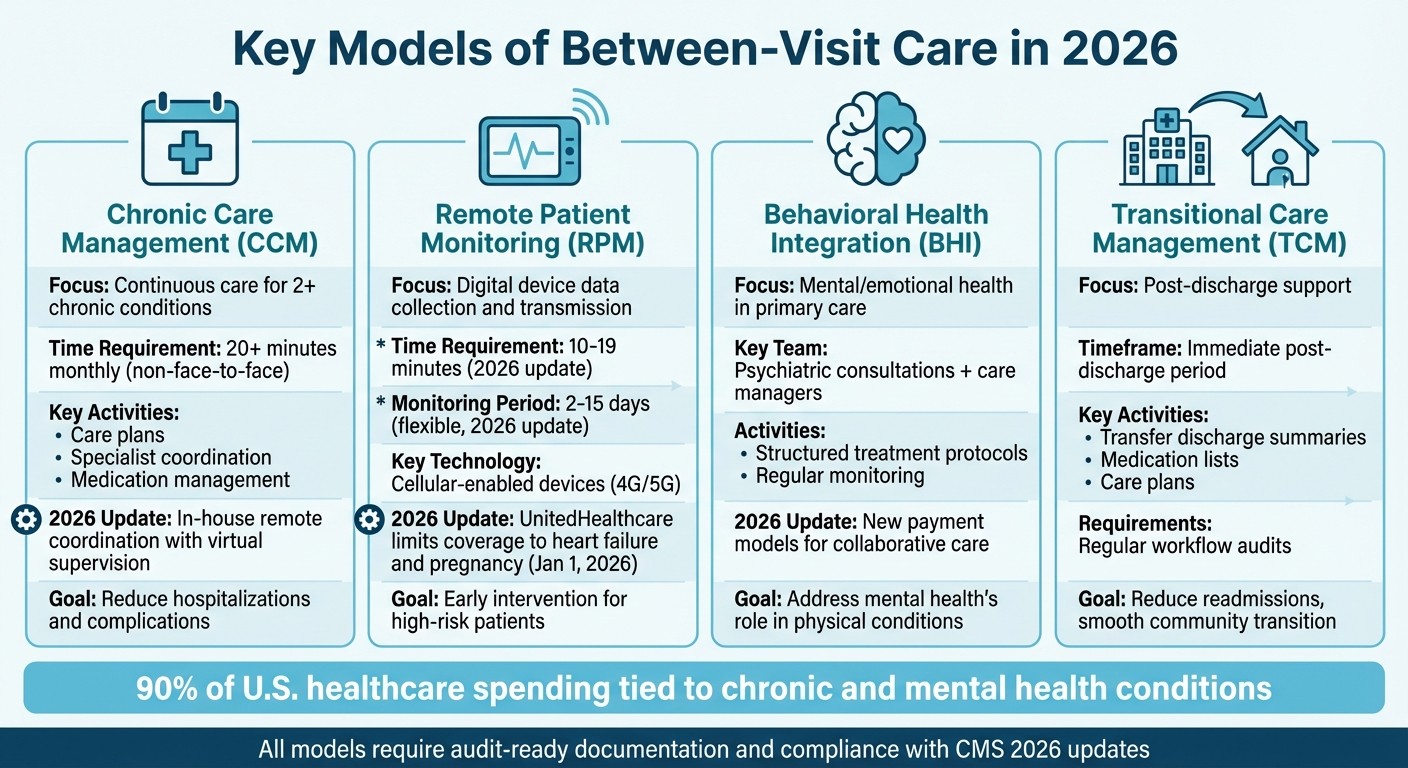
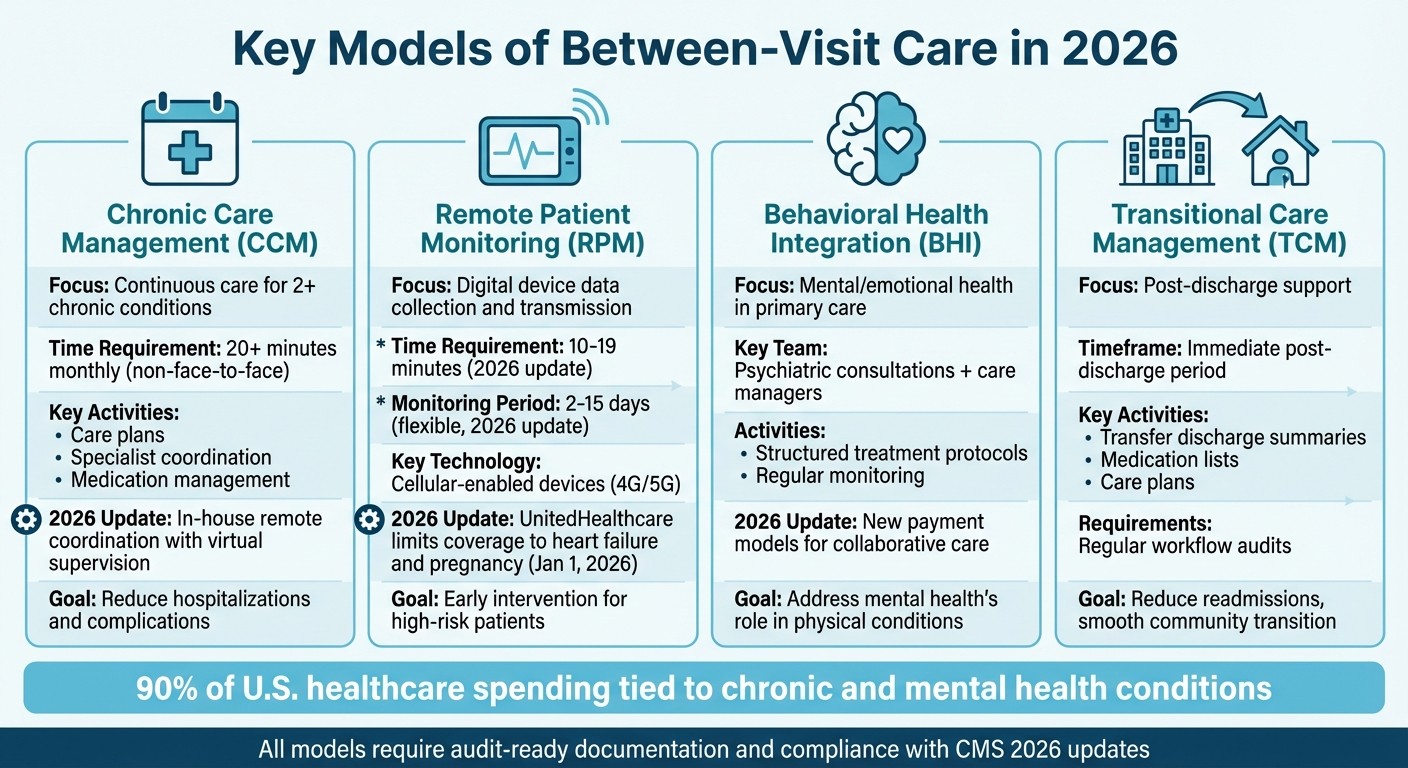
Four Key Between-Visit Care Models: CCM, RPM, BHI, and TCM Comparison 2026
Between-visit care includes several distinct approaches designed to meet specific patient needs. The primary models - Chronic Care Management (CCM), Remote Patient Monitoring (RPM), Behavioral Health Integration (BHI), and Transitional Care Management (TCM) - each have unique eligibility criteria, reimbursement structures, and compliance requirements. These models collectively highlight the ongoing evolution in healthcare as we approach 2026.
Chronic Care Management (CCM)
CCM focuses on providing continuous, proactive care for patients managing two or more chronic conditions. Unlike episodic care, CCM emphasizes activities that happen between office visits, such as creating comprehensive care plans, coordinating with specialists, and managing medications. These efforts aim to reduce complications and prevent hospitalizations.
Looking ahead to 2026, practices must ensure compliance with updated CMS eligibility criteria and maintain thorough documentation. CCM requires tracking at least 20 minutes of non–face-to-face care monthly, along with detailed records of all care coordination efforts. The latest updates encourage practices to adopt in-house remote care coordination with virtual supervision, enabling clinical teams to manage shorter, more frequent interactions effectively. This approach not only supports compliance but also helps improve long-term patient outcomes by reducing hospitalizations.
Remote Patient Monitoring (RPM)
RPM uses digital devices to collect and transmit physiological data, enabling early intervention and ongoing health monitoring. Cellular-enabled devices are a standout feature, as they reduce IT challenges by avoiding reliance on Wi-Fi connections. This continuous monitoring is particularly valuable for high-risk patients, allowing for timely responses and better health outcomes.
The 2026 CMS updates introduce new CPT codes to accommodate flexible monitoring periods (ranging from 2 to 15 days) and shorter interaction requirements (10 to 19 minutes). Additionally, UnitedHealthcare will limit RPM coverage to conditions like heart failure and pregnancy starting January 1, 2026. Practices must carefully review updated guidelines from CMS and commercial payors to ensure patient eligibility and compliance.
Behavioral Health Integration (BHI)
BHI brings mental and emotional health services into primary care, acknowledging the critical role mental health plays in managing physical conditions such as diabetes or heart disease. Behavioral health remains a leading area for telehealth, and the 2026 updates include new payment models to support collaborative care.
For successful implementation, practices must establish clear roles within virtual care teams to minimize confusion and ensure compliance. BHI programs typically involve regular psychiatric consultations, care manager support, and structured treatment protocols. Consistent documentation and monitoring are essential for maintaining program effectiveness and meeting compliance requirements.
Transitional Care Management (TCM)
TCM is designed to support patients immediately after discharge from a hospital or care facility, with the goal of reducing readmissions and ensuring a smooth transition to community-based care. This time-sensitive program focuses on the critical post-discharge period, emphasizing the seamless transfer of discharge summaries, medication lists, and care plans. Regular audits of workflows can help practices identify inefficiencies and address compliance concerns.
Key takeaways for 2026:
CCM emphasizes ongoing, coordinated care for patients with multiple chronic conditions, with a focus on continuity and compliance.
RPM utilizes cellular devices for continuous health monitoring, though coverage restrictions are tightening under some commercial insurers.
BHI integrates mental health into primary care, supported by updated payment models for collaborative care.
TCM provides focused, short-term support after hospital discharge to prevent readmissions and ensure effective transitions back to the community.
2026 Policy and Reimbursement Changes
As healthcare continues to shift toward between-visit care, staying informed about policy updates becomes essential for maintaining efficient operations. The Calendar Year 2026 Medicare Physician Fee Schedule (PFS) Final Rule, effective January 1, 2026, introduces reimbursement changes that directly impact Chronic Care Management (CCM), Remote Patient Monitoring (RPM), Behavioral Health Integration (BHI), and Transitional Care Management (TCM). For participants in qualifying Alternative Payment Models (APMs), the conversion factor increases to $33.57, while non-qualifying participants will see a slightly lower rate of $33.40. These adjustments will shape billing practices and bring heightened regulatory oversight.
CMS Reimbursement Updates
The 2026 PFS includes new RPM codes designed to address shorter monitoring periods (2 to 15 days) and reduced management times (10 to 20 minutes). These updates allow for more frequent billing, provided workflows are adjusted and documentation remains precise. However, overall payment increases are tempered by other changes, such as a -2.5% reduction in specific areas.
Compliance and Audit Requirements
CMS is increasing its focus on Medicare provider enrollment, introducing additional grounds for retroactive revocations and deactivations [8]. This heightened scrutiny means even minor documentation mistakes could trigger audits. Practices must prioritize maintaining audit-ready documentation to safeguard their billing and enrollment processes.
Value-Based Care Incentives
Alongside stricter compliance measures, CMS is updating quality measure incentives. For 2026, the Merit-based Incentive Payment System (MIPS) will feature 5 new quality measures and 3 new improvement activities, while 10 outdated measures and 8 activities will be removed. Practices focusing on chronic disease management, care coordination, and patient engagement can enhance their MIPS scores. These updates emphasize the importance of delivering consistent, patient-centered care that extends beyond the traditional office visit.
Technology for Scaling Between-Visit Care
Expanding between-visit care requires technology that simplifies workflows, reduces administrative tasks, and delivers actionable insights - all without overwhelming smaller clinical teams. Unified platforms serve as central hubs, seamlessly connecting electronic health records (EHRs), virtual care tools, health monitoring devices, and online pharmacy or lab portals into a single, streamlined system. By integrating these tools, healthcare teams can overcome fragmented systems and focus on delivering proactive, coordinated care. This technological foundation supports the development of more connected and efficient care solutions.
Unified Platforms for Workflow Integration
Fragmented systems often lead to duplicated efforts, missed follow-ups, and inconsistent care tracking. To ensure continuous, effective care, a unified system is crucial. These platforms bring together various programs into a single, cohesive workflow, reducing inefficiencies and enabling care teams to manage large patient populations more effectively. For example, OnCare360 integrates chronic care management, remote monitoring, transitional care, behavioral health services, medication reconciliation, and care gap tracking into one interface. This consolidation allows care teams to access patient histories, monitor interventions, and maintain audit-ready documentation - all without toggling between multiple systems or manually merging data. With unified workflows in place, advanced analytics can further enhance decision-making and care delivery.
AI-Driven Care Coordination
AI is reshaping between-visit care by analyzing patient data patterns, identifying potential health risks, and offering tailored care recommendations. In remote patient monitoring, AI-based platforms integrate with EHRs to provide real-time insights, automate routine tasks, generate structured notes, and streamline billing processes. This creates a collaborative model where AI highlights priorities, flags risks, and suggests documentation cues, while clinicians retain control over final decisions and care interventions. By reducing manual documentation and missed opportunities, this approach enables small clinical teams to efficiently manage larger patient panels.
Cellular Devices for Patient Monitoring
Consistent data transmission is essential for remote patient monitoring, particularly for patients in rural areas or those without reliable Wi-Fi. To address this, RPM systems must support various connectivity options, such as cellular (4G/5G) and Bluetooth, ensuring uninterrupted data flow regardless of location. Cellular-enabled devices simplify the process by eliminating technical barriers like app downloads, password resets, or home network configurations. These medical-grade devices integrate directly into care platforms, providing continuous monitoring for high-risk patients. This setup not only minimizes IT challenges but also facilitates earlier interventions, leading to improved patient outcomes.
Implementation Steps for Physician Practices
To successfully implement between-visit care, physician practices must align their patients' needs with compliant workflows and measurable outcomes. This involves assessing patient populations, creating detailed, audit-ready processes, and monitoring both clinical improvements and financial returns. The ultimate aim is to establish a program that grows sustainably without overloading staff or increasing compliance risks. These steps build on previously discussed care models to create a scalable and effective system for between-visit care.
Evaluating Patient Panels and Needs
Start by identifying care gaps, such as missed screenings, treatments, or follow-ups. Patients with multiple chronic conditions are particularly vulnerable to these gaps. For instance, medication non-adherence alone is linked to 125,000 deaths annually, with nearly 50% of chronic disease patients discontinuing medication refills within the first year of diagnosis.
Health Risk Assessments (HRAs), conducted during Annual Wellness Visits (AWVs), are invaluable tools for pinpointing patients who require between-visit support. These assessments can uncover missed opportunities for preventive care, such as pneumonia vaccinations, colorectal screenings, and mammograms. Beyond medical needs, practices should address social determinants of health by connecting patients to resources like pharmaceutical discounts, transportation services, food banks, and utility assistance. Programs like Chronic Care Management (CCM) provide dedicated care teams to maintain regular contact with patients, address real-time challenges, and coordinate care across both medical and social domains.
Creating Compliant Workflows
The CMS ACCESS Model, set to begin on July 1, 2026, represents a shift in Medicare reimbursement from fee-for-service to Outcome-Aligned Payments (OAPs), which reward practices for achieving measurable health outcomes. This model complements technology-driven solutions that streamline care delivery. To align with these changes, practices must develop workflows that can track and demonstrate clinical improvements, such as reducing blood pressure by 10 mmHg. Key performance metrics include condition-specific biomarkers like HbA1c, blood pressure, lipids, and weight, alongside Patient Reported Outcome Measures (PROMs) that assess pain, mood, and overall function.
Automating key processes - such as communication logs, time tracking, care plan documentation, and eligibility checks - ensures efficient and accurate documentation. Every patient interaction should include clear consent processes and meet audit-ready standards. Since ACCESS Model payments will be tied to the percentage of patients meeting defined outcome targets, precise documentation and outcome tracking are essential for optimizing revenue.
Tracking Outcomes and ROI
To validate the effectiveness of between-visit care, practices need to measure outcomes that demonstrate both clinical progress and financial returns. Key metrics include engagement rates, medication adherence, stability of vital signs, timeliness of interventions, reduced no-show rates, and fewer emergency department visits or acute care episodes. Additionally, tracking the revenue generated from CCM, RPM, and TCM services - as well as cost savings from reduced hospitalizations and improved chronic disease management - is crucial.
Real-time dashboards can help practices monitor monthly performance across patient panels. These tools allow teams to identify which interventions are achieving the best results and where workflows may need refinement. Sharing these insights with clinical staff, administrators, and payors highlights the tangible benefits of between-visit care. This transparency also positions practices to succeed in shared savings programs, capitation arrangements, and hybrid payment models as value-based care continues to expand.
Conclusion: Preparing for Between-Visit Care in 2026
This guide has highlighted the growing importance of proactive, between-visit care in reshaping practice operations. For physician practices aiming to excel within value-based care models, this shift is no longer optional. By 2026, CMS quality reporting will emphasize coordinated, patient-focused care that extends beyond traditional office visits. Practices will need to demonstrate measurable outcomes and consistent follow-through to align with these evolving standards. Those that embrace care beyond the clinic will be better equipped to thrive under CMS's redefined approach to value.
Technology plays a critical role in addressing these demands. Advanced care models driven by technology provide the tools needed for audit-ready documentation and compliance with CMS requirements. Practices that achieve strong compliance performance will benefit from fewer claim denials, more efficient audits, and operational improvements, which can lead to increased market share and profitability. Additionally, policymakers are expanding incentives tied to alternative payment models, linking reimbursement directly to outcomes and making technology indispensable for tracking and demonstrating progress.
To capitalize on these advancements, practices should adopt scalable workflows that meet compliance standards while enabling revenue capture from CCM, RPM, and TCM services. Integrating AI-powered care coordination, cellular monitoring devices, and robust documentation systems can ease operational challenges while enhancing clinical outcomes. These tools contribute to better management of chronic conditions, improved patient engagement, and stronger financial performance.
The time to act is now. Practices must assess their patient panels, close care gaps, implement compliant processes, and track measurable outcomes to secure revenue and maintain a competitive edge. Delaying these steps risks falling behind as CMS continues shifting reimbursement toward longitudinal, home-centered care models. By investing in the right infrastructure, physician groups can achieve better patient outcomes, reduced avoidable costs, and a stronger competitive position in the rapidly changing healthcare environment.
FAQs
What are the main benefits of between-visit care for managing chronic conditions?
Between-visit care plays a key role in managing chronic diseases by prioritizing consistent monitoring and timely interventions. This proactive approach helps patients avoid unnecessary emergency room visits and hospital admissions, contributing to better overall health outcomes. It also strengthens medication adherence and ensures smoother collaboration among healthcare providers, enhancing care coordination.
Another advantage is its ability to boost patient engagement. By involving patients more actively in their care, it fosters a sense of ownership and leads to improved long-term health results. For healthcare practices, between-visit care aligns seamlessly with value-based care objectives, supporting cost efficiency and enhancing financial performance.
What steps should practices take to stay compliant with CMS updates for between-visit care in 2026?
To align with the 2026 CMS updates, practices need to embrace integrated technology solutions that simplify compliance tasks. This includes automating documentation, monitoring care activities, and ensuring service requirements are consistently validated. Accurate record-keeping and smooth care transitions are essential to meet the new standards effectively.
Equally important is ongoing staff training on updated policies. Leveraging real-time audit tools and meticulously documenting every patient interaction can help practices stay on track with CMS guidelines. These measures not only support compliance but also enhance patient care, reinforcing the principles of value-based care.
How does technology help healthcare practices enhance between-visit care?
Technology plays a crucial role in transforming between-visit care by simplifying communication, enhancing care coordination, and supporting remote monitoring and telehealth services. It enables healthcare practices to exchange data effortlessly, automate repetitive tasks, and align workflows, ultimately making care delivery more efficient and focused on the patient.
Using tools such as remote patient monitoring (RPM), chronic care management (CCM), and behavioral health integration (BHI), healthcare teams can maintain consistent engagement with patients between visits. These tools help identify potential health concerns early and facilitate timely interventions. The result is not only improved patient outcomes but also greater operational efficiency and stronger financial performance within value-based care frameworks.

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects

Jan 5, 2026
CMS Updates: How RPM is changing in 2026

Jan 3, 2026
How AI Expands Care Coordinator Capacity

Jan 1, 2026
RPM Time Tracking Errors That Lead to Denials

Dec 31, 2025
CMS Consent Documentation: What Must Be Captured

Dec 30, 2025
Top 10 Documentation Errors in CCM & RPM

Dec 29, 2025
Audit-Ready Documentation: What CMS Expects
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?
Are you ready to explore the future of healthcare with OnCare360?
Contact us for more information or request a free consultation today.
Have questions?


